V-BID in Action: The Role of Cost-Sharing in Health Disparities
The existence of health disparities among specific populations has long been recognized; substantial variations in health insurance coverage, access to providers, use of specific clinical services, and patient-centered outcomes 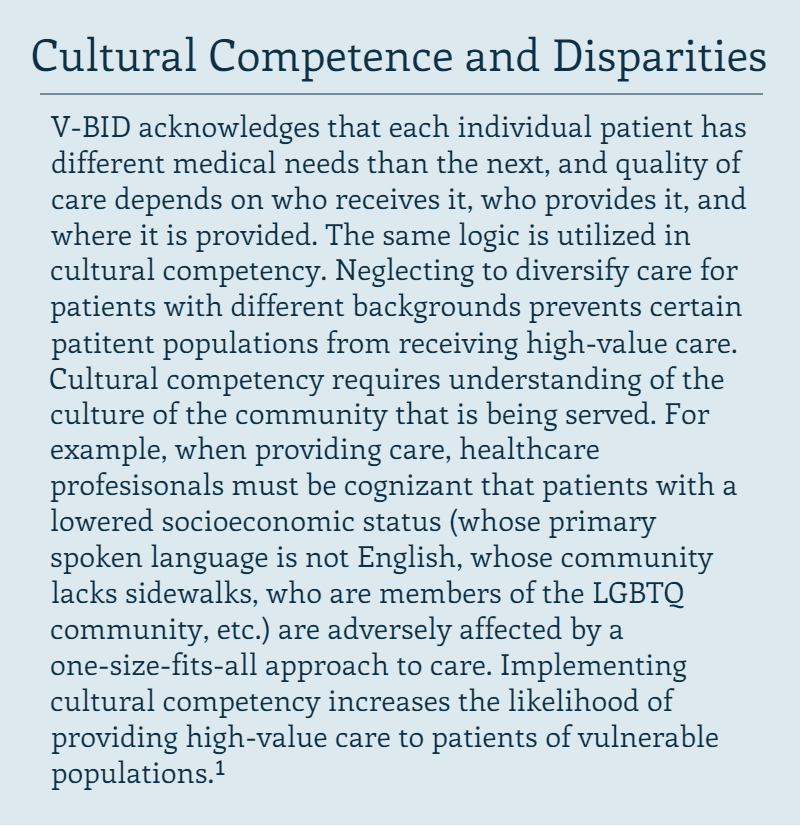 among different groups are well documented. Differences in levels of medical knowledge and information sources, trust and skepticism, participation, social support, and resources can vary significantly by population demographic. Adverse effects on health care equity have also been shown to be the result of clinician judgment, healthcare facility characteristics, and cultural milieu.
among different groups are well documented. Differences in levels of medical knowledge and information sources, trust and skepticism, participation, social support, and resources can vary significantly by population demographic. Adverse effects on health care equity have also been shown to be the result of clinician judgment, healthcare facility characteristics, and cultural milieu.
A robust evidence base has determined that the causes of these disparate outcomes are multifactorial; including race, ethnic group, income, education, and age. It is difficult to attribute blame to any single factor, as many of the predictors are inextricably linked.1
A systematic review of extensive published research documenting the scope of disparities and summary of proposed potential solutions are beyond the range of this brief. Our intention is to recognize a few critical factors contributing to disparities in health outcomes and provide examples of how each factor might impact utilization of evidence-based services once access to care is achieved. We propose that the removal of financial barriers to enhance utilization of high-value clinical services may be an effective approach in reducing disparities.
Race and Ethnicity
Race and ethnicity are frequently noted as important contributors to health disparities and have been documented to have an impact across the health care spectrum, from gaining access to care to the utilization of services once an individual engages with the health care system.
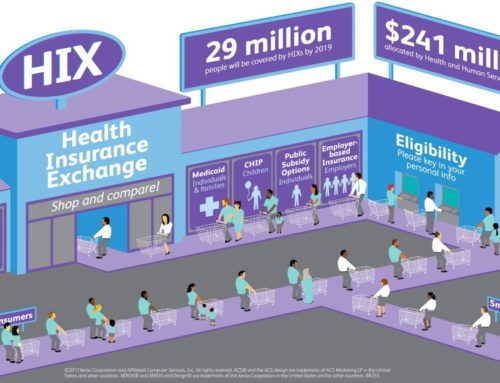
An increase in health insurance coverage attributable to the Affordable Care Act (ACA) has been substantial in White and Latino populations and has reduced the number of uninsured African-Americans by approximately 6.8%.11
Racial and ethnic disparities extend beyond access to care and have been demonstrated to persist after engagement with a health care provider. For example, it has been reported that members of Black and Hispanic households were more likely than White households to restrict the use of essential prescription medications due to cost.3 The self-reported health status of individuals who did not take their medications due to inability to pay was significantly lower than those who could afford to fill their prescriptions. This finding suggests that reducing cost-related non-adherence of high-value drugs can potentially improve patient-reported outcomes in vulnerable populations.
A study published by the American Journal of Managed Care has found that the removal of copayments largely eliminated racial disparities. In the study, the copayment for a statin drug used by patients with diabetes and vascular disease was reduced. Following this, there was a noted increase in medication adherence, leading the authors to call for additional research on the effect of V-BID has in reducing or eliminating racial disparities.12
Income and Education
Income and education have significant influences on health and are clearly interwoven with other factors that impact disparities. Individuals who live in poverty and have lower educational levels are more likely to be unemployed, without insurance, or enrolled in an insurance plan that does not offer full prescription coverage. They also have increased mortality rates and significantly worse self-reported health status.1 Chernew and colleagues demonstrated that individuals living in low-income areas are less adherent to essential medications and are more likely to be affected by increases in cost-sharing than those living in higher-income areas.4 This research suggests that targeted population-based programs that reduce financial barriers to care have the potential to increase utilization of high-value clinical services.
Age
The elderly are more likely to have lower incomes, poor health, and greater out-of-pocket spending on health care than non-elderly populations. This combination of factors places older Americans among the most vulnerable citizen groups. The assurance of Medicare coverage for those Americans 65 years of age and older detracts the focus of whether an insured beneficiary is able to access needed care.
Transportation concerns, literacy issues, cultural context, and out-of-pocket expenditures contribute to suboptimal outcomes even for those with Medicare coverage. For example, Trivedi and colleagues reported that when cost-sharing for clinician visits was increased, beneficiaries visited their doctors less frequently and spending on ambulatory care decreased.5 However, Medicare patients who were charged higher copays for doctor visits frequented the emergency department and were hospitalized more often than those whose cost-sharing did not increase, thereby leading to higher total costs. Moreover, the negative clinical and economic effects of increased cost-sharing were more pronounced in low-income individuals and beneficiaries with chronic illness.
As illustrated in the above example, the totality of published evidence strongly supports the notion that increases in consumer cost-sharing negatively affects vulnerable populations. The sentinel RAND Health Insurance Experiment (HIE) demonstrated that individuals who received free health care used more services than those who were required to pay for their health care, independent of health status. The HIE also found that the poorest and sickest members of the study population achieved better outcomes under the free plan in controlling hypertension, vision health, dental care, and reduction of symptoms for serious health conditions.6 The free plan also resulted in patients spending less time seeking medical care. The effect of cost-sharing on utilization was accentuated in the most vulnerable patients and indicates lowering out-of-pocket costs as a potential strategy to reduce disparities.
The Role for V-BID in Disparities
As consumers are being asked to pay an increasing portion of health care costs, cost-related non-adherence is a well-documented and increasingly important concern, particularly given its negative clinical impact on vulnerable populations. Value-Based Insurance Design (V-BID) is an innovative approach that can improve clinical outcomes and contain costs.7
V-BID reduces barriers to high-value clinical services and providers and discourages use of services and providers that are of lower value, aligning consumer out-of-pocket expenditures with value. V-BID is driven by the concept of clinical nuance, which recognizes that: (1) medical services differ in the benefit provided; and (2) the clinical benefit derived from a specific service depends on the patient using it, as well as when and where the service is provided. By incorporating greater clinical nuance into benefit design, payers, purchasers, taxpayers, and consumers can improve patient-centered outcomes, reduce disparities and bend the health care cost curve. V-BID argues that cost-sharing for high benefit services, such as preventive care, clinician visits, and medications used for the treatment of chronic disease should be kept low. V-BID programs that reduce copayments and coinsurance have been successfully implemented by private and public payers for individuals with chronic conditions such as diabetes, asthma, and heart disease. Accumulating evidence suggests that V-BID improves adherence, enhances clinical outcomes, and lowers consumer out-of-pocket contributions without an increase in total costs.8
Targeted copayment relief has the potential to shield low-income patients from the deleterious clinical effects of rising cost-sharing. A recent Health Affairs study concluded that the MI FREE program implementing V-BID principles reduced racial and ethnic disparities in health care. In the MI FREE study, commercially insured individuals who had experienced a myocardial infarction (i.e. heart attack) were randomly assigned to either usual prescription coverage or prescription coverage without cost-sharing for any generic or brand name angiotensin-converting enzyme (ACE) inhibitor, angiotensin receptor blocker, beta blocker, or statin. The enhanced prescription coverage group experienced improved medication adherence, lower rates of additional major vascular events, and decreased patient spending without increasing overall health costs.
A secondary analysis was performed to examine the effect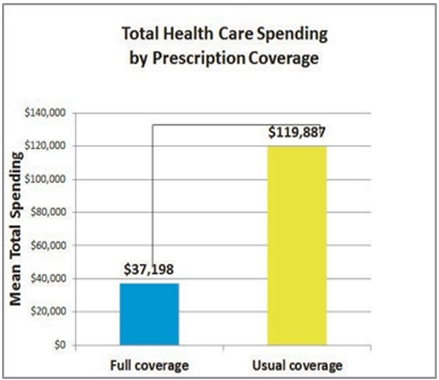 of the V-BID program on racial and ethnic disparities. At baseline, non-white patients enrolled in the MI FREE study were less adherent with prescribed medication and had higher health care spending than their white counterparts.9
of the V-BID program on racial and ethnic disparities. At baseline, non-white patients enrolled in the MI FREE study were less adherent with prescribed medication and had higher health care spending than their white counterparts.9
After cost-sharing was eliminated for the intervention group, adherence to beta-blockers and statins significantly improved for non-white enrollees, and a trend toward improved adherence for all three study medications was noted among non-white patients. Compared to non-whites with standard cost-sharing, non-white patients without cost-sharing experienced significantly lower readmission rates and a 70% reduction in total health care spending.
Conclusion
Despite the well-documented increases in out-of-pocket health care costs, disparities, and suboptimal patient-centered outcomes, Americans are being asked to shoulder a growing proportion of the health care cost burden. Cost-related non-adherence is a growing problem and has prompted a significant decline in self-reported health among vulnerable populations. The implementation of clinically nuanced V-BID programs with evidence-based services can improve quality of care, enhance the patient experience, lower costs, and reduce disparities.
References
1. Woolf SH, Braveman P. Where health disparities begin: The Role of Social and Economic Determinants and Why Current Policies may Make Matters Worse. Health Affairs. 2011; 30:(10): 1852M1859. Accessed at: http://content.healthaffairs.org/content/30/10/1852.full
2. Obamacare is Working. Unless You’re Black. Flavelle, Christopher. July 10, 2014, Bloomberg View. Accessed at: https://www.bloomberg.com/view/articles/2014-07-10/obamacare-is-working-unless-you-re-black
3. Heisler M, Langa KM, Eby EL, Fendrick AM, Kabeto MU, Piette JD. The Health Effects of Restricting Prescription Medication Use Because of Cost. Medical Care. 2004; (42):626M634. Accessed at: http://www.ncbi.nlm.nih.gov/pubmed/15213486
4. Chernew M, Gibson TB, YuMIsenberg K, Sokol MC, Rosen AB, Fendrick AM. Effects of Increased Patient Cost Sharing on Socioeconomic Disparities in Health Care. Journal of General Internal Medicine. 2008; 23(8):1131–6 . Accessed at: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2517964/
5. Trivedi AN, Moloo H, Mor V. Increased Ambulatory Care Copayments And Hospitalizations Among The Elderly. New England Journal of Medicine. 2010;362(4):320M28. Accessed at: http://www.nejm.org/doi/full/10.1056/NEJMsa0904533#t=article
6. http://www.rand.org/pubs/research_briefs/RB9174.html
7. Chernew ME, Rosen AB, Fendrick AM. Value-Based Insurance Design. Health Affairs. 2007;26(2):195–203. Accessed at: http://content.healthaffairs.org/content/26/2/w195.abstract
8. http://vbidcenter.org/the-evidence-for-v-bid-validating-an-intuitive-concept/
9. Choudhry NK, Bykov K, Shrank,WH, Toscano M, Rawlins W, Reisman L, Brennen TA, and Franklin JM. Eliminating Medication Copayments Reduces Disparities in Cardiovascular Care, Health Affairs. 2014; 33(5): 863M870. Accessed at: http://content.healthaffairs.org/content/33/5/863.abstract
10. Choudhry NK, Avorn J, Glynn RJ, Antman EM, Schneeweiss S, Toscano M, et al. Full Coverage For Preventive Medications After Myocardial Infarction. New England Journal of Medicine. 2011; 365(22):2088–97. Accessed at: http://www.nejm.org/doi/full/10.1056/nejmsa1107913#t=article
11. Secretary, HHS Office of the. “The ACA Is Working for the African-American Community.” HHS.gov. Assistant Secretary for Public Affairs, Web. 17 Aug.2016. Accessed at: http://www.hhs.gov/healthcare/facts-and-features/fact-sheets/aca-working-african-american-community/
12. Lewey, Jennifer, MD, William H. Shrank, MD, MSHS, Jerry Avorn, MD, Jun Liu, MD, MPH, and Niteesh K. Choudhry, MD, PhD. “Medication Adherence and Healthcare Disparities: Impact of Statin Co-Payment Reduction.”AJMC. American Journal of Managed Care, 09 Oct. 2015. Web. 17 Aug. 2016. Accessed at: http://www.ajmc.com/journals/issue/2015/2015-vol21-n10/medication-adherence-and-healthcare-disparities-impact-of-statin-co-payment-reduction
13. Betancourt, Joseph R., Alexander R. Green, J. Emilio Carrillo, and Elyse R. Park. “Health Affairs.” Cultural Competence And Health Care Disparities: Key Perspectives And Trends. Health Affairs, 1 Mar. 2005. Web. 17 Aug. 2016. Accessed at: http://content.healthaffairs.org/content/24/2/499.abstract
14. Gayer, Matt. “Take a Two-step Approach to Reducing Health Disparities.” Advisory Board. Advisory Board, 21 June 2016. Web. 17 Aug. 2016. Accessed at: https://www.advisory.com/research/care-transformation-center/care-transformation-center-blog/2016/06/cultural-competency-two-phase