When it comes to the political iceberg of drug costs, there is more than meets the eye. Policies that reduce overall cost but do not lower consumers’ out-of-pocket costs will not address the main challenge facing most Americans.
Access to affordable prescription drugs is a topic of increasing public concern. In a recent survey, 82% of respondents identified medical costs as their biggest financial challenge. Although prescription spending growth has moderated and drug spending remains a relatively small part of total medical expenditures, a 2018 Kaiser Family Foundation poll showed that a significant majority of Americans think that Congress and the president are not doing enough about the problem.
Before policies exclusively aimed at lowering drug costs are implemented, the clinical and financial effects of drugs should be carefully scrutinized relative to available alternatives. Importantly, the value created by a specific drug—preferably determined for a specific clinical indication—should be compared not only with other pharmaceuticals, but also with non-drug services. Cost is only part of the value equation. Rigorous assessments of clinical services have concluded that certain expensive drugs are of extremely high value, whereas some commonly used diagnostic tests, procedures, and inexpensive drugs are of no value and are even harmful.
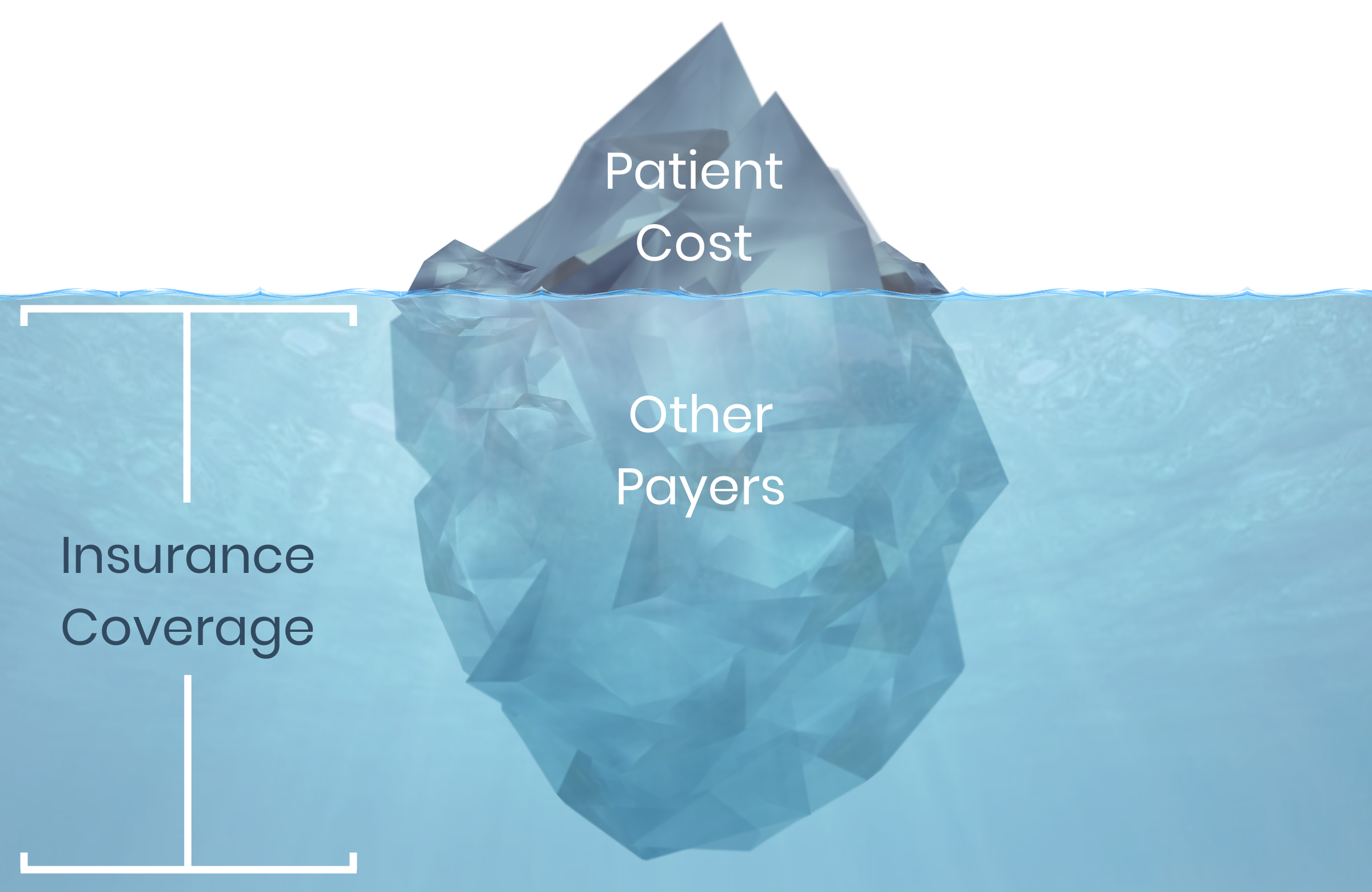
The Drug Cost Iceberg
As stakeholders wrestle with the complex issue of pharmaceutical costs, it is important to consider 2 separate components of drug costs: (1) the cost paid by the patient (ie, out-of-pocket costs) and (2) the remaining portion paid by other payers (eg, insurance companies). American Patients First: The Trump Administration Blueprint to Lower Drug Prices and Reduce Out-of-Pocket Costs, published in May 2018, explicitly acknowledged this important distinction.
The Drug Cost Iceberg illustrates that the acquisition cost is partially paid for by consumers (the part of the iceberg above the water) and a portion by third parties (the part below the surface), such as the government or an employer. Current policy initiatives under consideration mainly address the total cost paid for the drug—the entire iceberg. Most of these proposals are politically contentious and, if enacted, would be unlikely to address the public’s desire to lower out-of-pocket costs (reducing the iceberg tip) in the near future.
There is an immediate urgency to provide patients with relief from out-of-pocket costs for their medications. Although health plans pay for an increasing proportion of drug expenditures, the absolute amount paid by patients has grown as well. A robust evidence base confirms that medication adherence declines as patients are required to pay more to fill their prescriptions. One in four Americans report difficulty affording their prescriptions; cost-related non-adherence occurs more frequently among individuals who are economically disadvantaged and/or diagnosed with multiple chronic conditions. This problem is expected to worsen as more Americans are enrolled in a health plan that includes a deductible. These individuals must pay the total cost of their prescriptions until the full amount of the plan deductible is met (ie, patients pay for the entire iceberg).
The ‘True Value’ Iceberg
 A perilous (and likely long) journey to reduce total drug acquisition costs is unlikely to enhance consumers’ access to affordable medications in the near future. While these ambitious “melt the entire iceberg” proposals are deliberated, it is important to simultaneously consider initiatives that reduce the patient financial burden (ie, shrink the tip). Programs that reduce patient cost sharing for essential medications (eg, value-based insurance design), as well as regulatory changes such as allowing health savings accounts/high-deductible health plans the flexibility to cover medications that treat chronic diseases on a pre-deductible basis, have broad multi-stakeholder and rare bipartisan political support. These initiatives would be feasible for plans to implement and could quickly lower out-of-pocket drug costs for tens of millions of Americans with chronic conditions.
A perilous (and likely long) journey to reduce total drug acquisition costs is unlikely to enhance consumers’ access to affordable medications in the near future. While these ambitious “melt the entire iceberg” proposals are deliberated, it is important to simultaneously consider initiatives that reduce the patient financial burden (ie, shrink the tip). Programs that reduce patient cost sharing for essential medications (eg, value-based insurance design), as well as regulatory changes such as allowing health savings accounts/high-deductible health plans the flexibility to cover medications that treat chronic diseases on a pre-deductible basis, have broad multi-stakeholder and rare bipartisan political support. These initiatives would be feasible for plans to implement and could quickly lower out-of-pocket drug costs for tens of millions of Americans with chronic conditions.
When it comes to the political iceberg of drug costs, there is more than meets the eye. Policies that reduce overall cost but do not lower consumers’ out-of-pocket costs will not address the main challenge facing most Americans. Implementation of practical strategies that reduce out-of-pocket costs—shrinking the tip—are warranted to help struggling Americans afford their essential medications and ultimately improve their health.