REDUCING NO-VALUE CARE TO
ENHANCE HEALTH EQUITY
It is well documented that populations of color and low-income individuals are less likely to receive the clinical services that play a critical role in preventing and managing disease. A more recent and growing evidence base suggests that underserved communities are also at risk of receiving more low-value care, defined as services that provide little or no benefit to patients, have potential to cause harm, incur unnecessary costs to patients, and/or waste limited health care resources. This misallocation highlights the shortcomings of the existing health care delivery infrastructure leading to inequities in access to effective clinical care and disparities in patient-centered outcomes. Therefore, efforts to improve health equity that focus exclusively on promoting access to high-value care overlook an important contributing component. Thus, initiatives aimed to reduce disparities should simultaneously aim to reduce low-value care. A starting point for this work could be identifying and reducing the use of ‘no-value care’ among disadvantaged populations, services for which there is rigorous evidence demonstrating no clinical benefit in specific clinical scenarios and minimal/no patient demand.
Despite spending more on health care per capita than any other country, the United States medical care system underachieves in delivering on patient-centered outcomes and population health metrics. Previous studies estimated that up to 1/3 of total U.S. health care expenditures are spent on services that do not contribute to individual or population health [1]. While the receipt of low-value care (LVC) is a burden to individuals – and society at large – with respect to time, risk, and efficient use of resources, the negative impact is disproportionally borne by individuals with lower opportunity for good health.
Disparities in health care exist at the intersections of race and ethnicity, sexual orientation and gender identity, age, geography, and many other factors. Racism and discrimination in policy design, implementation, and evaluation at the federal, state, and local levels have led to structural social and economic suppression, unequal education access, and residential segregation [2]; all of which contribute to lower rates of health care access and coverage, higher rates of mortality and morbidity, and poorer health outcomes and health care quality for people of color [3].
While health system performance scores vary widely among states, one consistent finding across nearly all states is that White people receive more and better care when compared to other racial groups [4]. Thus, addressing disparities in health and medical delivery to ensure that all Americans have the opportunity for good health is important not only from a social justice and equity standpoint, but also for improving the nation’s overall wellbeing and economic prosperity [5].
Low-Value Care
Racial and ethnic disparities in access to effective care have been studied extensively, but only recently have research efforts begun to focus on whether these disparities extend to the receipt of low-value care, defined as services that provide little or no benefit to patients, have potential to cause harm, incur unnecessary costs to patients, or waste limited health care resources. For example, in a 2017 analysis of Medicare administrative data, Schpero and colleagues reported that receipt of low-value care among Black and Hispanic beneficiaries was often demonstrably higher, compared with White beneficiaries [6].
A decade ago, drawing upon medical professionalism to trigger conversations between patients and clinicians about potentially overused services, the Choosing Wisely campaign was launched, ultimately identifying more than 600 low-value diagnostic tests, treatments, and services specified by more than 80 professional societies. Despite educational campaigns, an intense research focus, and initiatives designed to curb LVC and wasteful spending, expenditures on LVC by private and public payers have decreased only marginally [7].
No-Value Care: An Actionable Subset of Low-Value Care
One reason for the minimal progress is the lack of an actionable LVC definition that directly addresses the value of a specific medical service, which depends on several factors, including interpretation of the available evidence in specific clinical scenarios, as well as patient preferences. Thus, to promote the success of existing and future efforts to drive the U.S. towards a value-based system, it may be more effective to start with ‘low-hanging fruit’ by identifying unnecessary services with minimal elements left to interpretation (i.e. available evidence in specific clinical scenarios, patient preferences, etc.) among interested stakeholders [8].
The use of no-value care services in specified populations and specific clinical scenarios does not improve clinical outcomes, and in many cases reduces patient satisfaction and causes harm.
Accordingly, a more actionable subset of low-value care – or “No-Value Care” (NVC) – could be identified to move this important agenda forward. The use of these NVC services in specified populations and specific clinical scenarios does not improve clinical outcomes (at best), and in many cases reduces patient satisfaction and causes harm (at worst) [1].
No-value care is defined as meeting the following criteria:
- Rigorous evidence demonstrates no clinical benefit, or that the clinical harms outweigh the benefits (i.e., no net benefit) when used in specific clinical circumstances by defined patient populations
- This must not conflict with expert consensus or clinical guidelines for defined patient populations or override physician-patient decisions about the best treatment for an individual patient
- No/low variability in net clinical benefits based on patient characteristics or clinical scenario (such as age, sex, disease severity, site of lesion, evolving diagnostic criteria, changes in standard care, time-dependent care, differences in baseline risks, and dose-dependent effects)
- No/low variability in patient preferences [8]
Expenditures on NVC compound health care disparities by potentially diverting spending away from high-value care and investment in other factors impacting health disparities. The drivers behind the use of no-value care are complex, including misaligned financial incentives, defensive medical practice, deference to patient requests for testing or treatment, non-evidence-based clinical heuristics, and clinical practice cultures that encourage excessive care [9]. Examples include those services that receive a D rating from the United States Preventive Services Taskforce [10], for which “there is a moderate of high certainty that the service has no net benefit or that the harms outweigh the benefits” (Table 1). While USPSTF D-rated services are a potential starting point to identify NVC services, it may not fully capture the full range of NVC services persistent in the U.S. health care system.
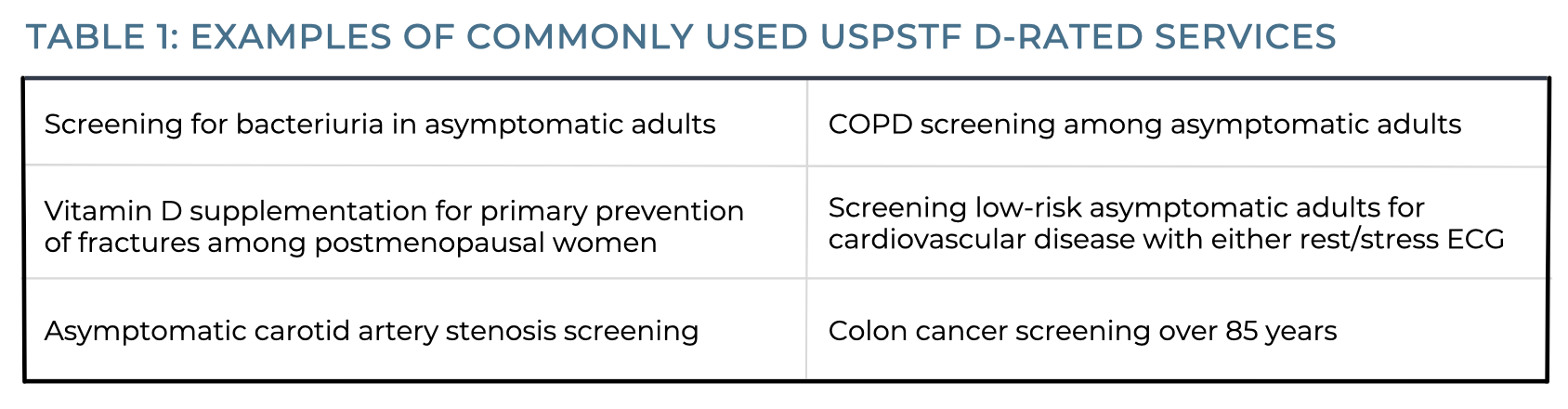
Analyses show that Medicare beneficiaries received the 6 commonly used USPSTF D-rated services in the table above over 30 million times per year, leading to over $600 million in wasteful spending annually [11,12]. Moreover, the use of these and other NVC services poses the risk of triggering cascades of additional care – subsequent clinician visits, diagnostic tests, and procedures [9]. For example, for every dollar spent by the Medicare program for prostate cancer screening for men older than 70 years of age, an additional six dollars is spent on follow up care [13].
REDUCING NO-VALUE CARE AND ENHANCING EQUITY IN COMMUNITIES OF COLOR
Multiple state and federal health care stakeholders, including benefit exchanges, health plans, and actuaries are designing and implementing policies and programs that incorporate an equity lens in health care delivery. Examples include: the District of Columbia Health Benefit Exchange has established a Social Justice and Health Disparities Working Group to improve access to high-value services for clinical conditions that disproportionally impact populations of color (e.g., diabetes, pediatric mental health) [14]; the National Association of Insurance Commissioners has established a special committee on race and insurance [15]; and the American Academy of Actuaries health equity work group [16]. These efforts that explicitly address the reality that underserved populations receive a disproportionate amount of unnecessary care, coupled with ongoing multi-stakeholder initiatives (e.g. Starfield Summit V) that classify actionable lists of NVC services, can inform policies generating substantial savings, which could be reallocated to spending on higher-value care. Such a patient-centered redistribution of medical spending would improve individual and population health, enhance equity and ensure more efficient health care expenditures.
University of Michigan Center for Value-Based Insurance Design
The University of Michigan Center for Value-Based Insurance Design (V-BID Center) is the leading advocate for development, implementation, and evaluation of clinically nuanced health benefit plans and payment models. Since 2005, the Center has been actively engaged in understanding the impact of innovative provider facing and consumer engagement initiatives, and collaborating with employers, consumer advocates, health plans, policy leaders, and academics to improve clinical outcomes and enhance economic efficiency of the U.S. health care system.
Funding for this V-BID Center Brief was provided by PhRMA.
REFERENCES
- Shrank WH, Rogstad TL, Parekh N. Waste in the US Health Care System – Estimated Costs and Potential for Savings. JAMA. 2019;322(15):1501-1509.
- Smedley BD, Stith AY, Nelson AR. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. 2003. DOI: 10.17226/12875.
- Serchen J, Doherty R, Atiq O, Hilden D. A Comprehensive Policy Framework to Understand and Address Disparities and Discrimination in Health and Health Care: A Policy Paper From the American College of Physicians. Ann Int Med. 2019.
- Ndugga N, Artiga S. Disparities in Health and Health Care: 5 Key Questions and Answers. KFF. 2021.
- Radley DC, Baumgartner JC, Collins SR, Zephyrin L, Schneider EC. Achieving Racial and Ethnic Equity in U.S. Health Care. The Commonwealth Fund. 2021.
- Schpero WL, Morden NE, Sequist TD, Rosenthal MB, Gottlieb DJ, Colla CH. For Selected Services, Blacks and Hispanics More Likely To Receive Low-Value Care Than Whites. Health Affairs. 2017.
- Cliff BQ, Advanceña ALV, Hirth RA, Daniel Lee SY. The Impact of Choosing Wisely Interventions on Low-Value Medical Services: A Systematic Review. Milbank Q. 2021.
- Fendrick AM, Neumann PJ, Beaudin-Seiler B. No-Value Care: A Starting Point to Reduce Wasteful Healthcare Spending. Research Consortium for Health Care Value Assessment. 2022.
- Kini V, Breathett K, Groeneveld PW, Ho PM, Nallamothu BK, Peterson PN, Rush P, Wang TY, Zeitler EP, Borden WB. Strategies to Reduce Low-Value Cardiovascular Care: A Scientific Statement From the American Heart Association. Circ Cardiovasc Qual Outcomes. 2022.
- USPSTF Grade Definitions.
- Oronce CIA, Fendrick AM, Ladapo JA, Sarkisian C, Mafi JN. The Utilization and Costs of Grade D USPSTF Services in Medicare, 2007-2016. J Gen Intern Med. 2021.
- Schwartz AL, Landon BE, Elshaug AG, et al. Measuring Low-Value Care in Medicare. JAMA Intern Med. 2014.
- Kim DD, Daly AT, Koethe BC, et al. Low-Value Prostate Specific Antigen Test for Prostate Cancer Screening and Subsequent Health Care Utilization and Spending. JAMA New Open. 2022.
- Lewis DC. Washington, D.C.’s State-Based Marketplace Is Addressing Health Disparities And Systemic Racism In Health Care. Health Affairs Forefront. 2022.
- NAIC Special (EX) Committee on Race and Insurance – Adopted Changes.
- American Academy of Actuaries – Health Equity Committee.