Supporting Consumer Access to Specialty Medications through Value-Based Insurance Design
Originally Produced: June 2014 Updated: February 2017
Introduction
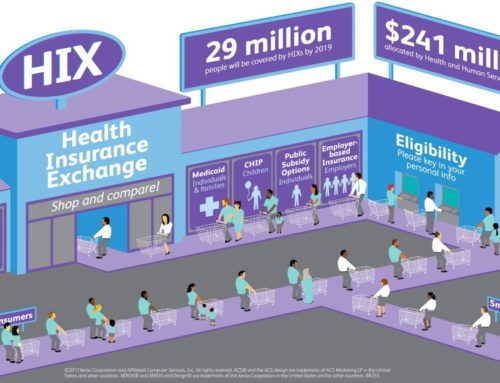
Specialty pharmaceuticals are medications that consist of complex molecules, are often complicated to deliver, and/or carry high costs. These medications are frequently used in the treatment of rheumatoid arthritis (RA), HIV, multiple sclerosis (MS), cancer and a variety of other serious health conditions. For many patients, specialty medications represent the most appropriate clinical recommendation. However, the benefit delivered by any given medication may vary markedly depending on the particular circumstances around its use. Today, approximately a quarter of total pharmaceutical spend-ing in the commercial market is devoted to specialty medications. If current trends in utilization hold, it is estimated that spending on specialty medications will comprise half of all pharmaceutical expenditures by 2018.1
To constrain the rapid rate of increased spending, many payers have established high consumer cost-sharing requirements for these medications. To address the clinical and economic effects of higher cost sharing for specialty medications, the Center for Value-Based Insurance Design, in collaboration with the National Pharmaceutical Council, has issued a white paper supporting consumer access to specialty medications. Value -Based Insurance Design (V-BID) is an innovative approach that can improve clinical outcomes and contain costs. V-BID reduces barriers to high-value clinical services and providers and discourages use of services and providers that are of lower value, aligning consumer out of pocket expenditures with value. V-BID is driven by the concept of clinical nuance which recognizes that: (1) medical services differ in the benefit provided; and (2) the clinical benefit derived from a specific service depends on the patient using it, as well as when and where the service is provided. By incorporating greater clinical nuance into benefit design, payers, purchasers, taxpayers, and consumers can attain more health for every dollar spent.
Consequences of High Cost-Sharing for Specialty Medication
Until 2002, most individuals with employer-sponsored insurance with prescription drug coverage were in plans with one or two formulary tiers. However, in 2013, nearly 1 in 4 insured individuals were in plans with four or five tiers, with tiers four and five typically devoted to specialty medications.2 Of those in plans with specialty tiers, more than 40% were subject to coinsurance-based (rather than copayment-based) cost-sharing.3 The average coinsurance rate for specialty tier drugs is about 30%, although coinsurance rates as high as 50% exist. This strategy of increased consumer cost-sharing may trigger cost-related non-adherence for some patients leading to more complicated and expensive medical interventions and correspondingly adverse results for payers. Instead, of “one size fits all” cost sharing increases, payers and purchasers should consider implementing utilizing value-based insurance design (V-BID) to assure that patients have access to necessary specialty medications.
It is well-documented that as cost-sharing for health care services increases, medication initiation and adherence decreases for both essential and non-essential therapies.4 For some conditions, the appropriate use of specialty medications may avert emergency room visits and hospitalizations. These savings may offset increased spending on pharmaceuticals and may offer savings to the employer related to workplace productivity. For example, a 2009 analysis found that the cost to employers of lost productivity due to poor health is 2.3 times as much as the cost of direct medical and pharmacy spending combined.3 For three conditions commonly treated with specialty pharmaceuticals—rheumatoid arthritis (RA), multiple sclerosis (MS), and cancer—a substantial body of research shows that cost-related non-adherence is a significant issue associated with increased morbidity, and for some conditions, increased mortality.5
Applying V-BID to Specialty Medication
V-BID principles can be applied to align specialty medications and appropriate populations by basing consumer cost-sharing on a drug or treatment’s clinical value, not acquisition cost. Implementing a V-BID prescription specialty medication plan that offers clinically nuanced cost-sharing based on patient-or disease-specific characteristics and that directs consumers toward high-value providers, payers, and purchasers can improve consumers’ access to necessary medications and reduce the likelihood of missed or delayed care and appropriate utilization of specialty medications.
Impose Only Modest Cost-Sharing on High-Value Medications
Abolishing the elaborate four- and five-tier ranking system and related intricate cost-sharing formula may be the most direct approach to promoting access to all medically necessary treatments. Such an approach limits possibilities for differentiation among treatments within the tiers, but promotes access to all potentially important medications. The approach is required in state-regulated plans in New York6 and Vermont7. Payers and purchasers may also become more selective by lowering cost-sharing for certain chosen specialty drugs. A payer or purchaser, in partnership with physician leaders, can identify particular specialty medications that consistently deliver outstanding value given prescribing patterns. These drugs can be moved to lower tiers with reduced cost-sharing requirements. A similar approach could be used when evidence suggests that non-adherence among a particular population is especially problematic.
Reduce Cost-Sharing in Accordance With Patient- or Disease-Specific Characteristics
Payers and purchasers should consider reducing cost-sharing for specialty drugs on the basis of patient characteristics when evidence suggests that the therapy is especially important to achieve optimal health outcomes. For example, among cancer patients, the type of cancer, the stage of chemotherapy, and the presence or absence of a biomarker (a biological indicator used to determine risk, estimate prognosis, select optimal therapy, etc.) frequently can be referenced to differentiate high-value treatment from low-value treatment.
Relieve Patients from High Cost-Sharing After Failure on a Different Medication
Reducing cost-sharing for specialty medications if the patient does not respond as desired to another medication is another strategy. For example, a payer might wish to encourage the use of methotrexate as a first-line treatment for RA, given reasonable levels of effectiveness in certain patients. However, not all patients respond adequately to therapy with only this medication.
A “reward the good soldier” V-BID benefit structure would relieve a patient from higher cost-sharing for biologics (e.g., adalimumab, etanercept) after failure of the more preferred regimen.
Use Cost-Sharing to Encourage Patients to Select High-Performing Providers and Facilities
Payers and purchasers can encourage consumers to select high-value settings and providers through differentiated cost-sharing. Plans can offer lower cost-sharing to direct consumers to high-value providers, for those members choosing to receive care at sites that meet one or more of the following characteristics related to quality and efficiency:
- Designation as a “center of excellence”;
- Consistent use of evidence-based clinical pathways, such as National Comprehensive Cancer Network (NCCN) guidelines for cancer patients, with an allowance for deviation based on individual circumstances;8
- Tendency to appropriately engage patients in key decisions;
- Tendency to avoid costly services when their use will not affect treatment decisions; and
- Consistency in achieving key condition-specific quality goals.
Keys to Success
Successful implementation of clinically nuanced benefit designs for specialty pharmaceuticals will require addressing several challenges. These include:
- Preparing for administrative complexity;
- Establishing incentives that engage patients early;
- Communicating effectively about V-BID;
- Integrating V-BID with provider-facing initiatives; and
- Recognizing that perfect must not be the enemy of good.
Conclusion
Payers and purchasers must be cognizant of how cost-sharing can impact adherence, health, productivity, and financial well-being among all patients who use specialty medications. Given the prevalence of four- and five-tier arrangements that incorporate high levels of cost-sharing, the potential for harm due to non-adherence is particularly significant for patients with conditions that are managed with high-tier specialty medications. V-BID principles can improve quality, reduce waste, foster engagement, and mitigate legitimate concerns that one-size-fits-all cost-sharing may lead individuals to forgo clinically important care. Using V-BID principles to align clinical effectiveness with overall value, and in turn, cost-sharing, ensures clinical effectiveness at the right price.
References:
- Express Scripts drug trend report. Express Scripts Web site. The 2013 Drug Trend Report. Published 2014. Accessed April 16, 2014.
- Kaiser Family Foundation, Health Research & Educational Trust. Employer health benefits 2013 annual survey. http:// kaiserfamilyfoundation.files.wordpress.com/2013/08/8465-employer-health-benefits-20131.pdf. Published 2013. Accessed April 16, 2014.
- Loeppke R, Taitel M, Haufle V, Parry T, Kessler RC, Jinnett K. Health and productivity as a business strategy: a multiemployer study. J Occup Environl Med. 2009;51(4):411-428.
- Goldman DP, Joyce GF, Zheng Y. Prescription drug cost sharing: associations with medication and medical utilization and spending and health. JAMA. 2007;298(1):61-69.
- http://vbidcenter.org/wp-content/uploads/2014/10/vbid-specialty-medications-npc2014-final-web.pdf
- An act to amend the public health law and the insurance law, in relation to cost-sharing, deductible or co-insurance for tier IV prescription drugs; and to amend the executive law, in relation to unlawful discriminatory practice in relation to tier IV prescription drugs. S5000. 2009-2010 Reg Sess (NY 2010). http://assembly.state.ny.us/leg/?sh=printbill&bn=S05000&term=2009. Accessed April 16, 2014.
- An act relating to modifications to the ban on gifts by manufacturers of prescribed products. Act 51. 2011-2012 Leg Sess (VT 2011). http://www.leg.state.vt.us/docs/2012/Acts/ACT051.pdf. Accessed April 16, 2014.
- National Comprehensive Cancer Network. NCCN Guidelines® and derivative information products: user guide. http://www.nccn.org/ professionals/. Published 2014. Accessed April 16, 2014.