Value-Based Insurance Design: Contributions to Consumer Health in Consumer-Directed Health Plans1
Value-Based Insurance Design: Contributions to Consumer Health in Consumer-Directed Health Plans1
Originally Produced: April 2012. Updated: June 2016
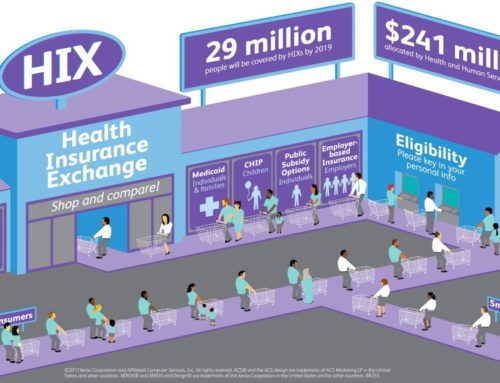
A consumer-directed health plan (CDHP) is an insurance product that offers lower premiums in exchange for higher patient deductibles than traditional plans. People who use CDHPs are responsible for paying for most of their routine care. The goal of CDHPs is to make customers more cost-conscious about the care they use, theoretically saving money on foregone services and lowering prices for consumers. In 2010, 28 million people were enrolled in a CDHP; in the same year nearly half of all employers reported that they planned to offer a CDHP to their employees within five years.2
CDHPs have faced criticism because the higher deductibles may cause patients to use less care. Research shows that when cost sharing is increased, consumers will forgo needed as well as unneeded care, and are likely to have poorer health as a result.3,4,5,6 CDHP consumers with chronic diseases or low incomes are more likely to be impacted by higher out-of-pocket costs, and to have worse clinical outcomes if they avoid care.7
Value-Based Insurance Design Waiver
In order to mitigate the negative health effects that may result from increased cost sharing for high-value health care, the Center for Value-Based Insurance Design (V-BID Center) recommends that insurers add an evidence-based “V-BID waiver” to high deductible plans by instituting lower or no cost-sharing for clinically proven health care. Many services that are designated as health care quality metrics require high patient deductibles in most CDHP plans.8 V-BID is an innovative and widely implemented approach to providing health benefits that seeks to enhance patients’ clinical outcomes and constrain health care cost growth. By reducing barriers to high-value, evidence-based services and providers (often through lower costs and other patient incentives) V-BID plans can achieve improved health outcomes at any level of health care expenditure. A V-BID waiver program would ensure that consumers are not deterred from receiving needed treatment (high-value care), while preserving disincentives to care without demonstrated effectiveness (low-value care), enhancing the quality of CDHPs while preserving the overall affordability of the plans.
The key to a V-BID program is clinical nuance. V-BID programs target high-value treatments, services, and medications, and lower barriers across the entire continuum of clinical care. Studies show that when barriers to high-value care are reduced, patient compliance with recommended treatments increases and potential cost savings result.9,10 Numerous treatments and services have already been identified for disease management programs, pay-for-performance initiatives, and health plan accrediting organizations such as the National Committee for Quality Assurance. A hybrid plan design, “the high-value low-deductible health plan,” combines the V-BID premise of removing patient barriers to high-value care with market-driven consumer incentives that are the foundation of CDHPs.
Steps to Promoting Needed and Valuable Care
A major step toward aligning consumer costs with services’ value was taken when the Patient Protection and Affordable Care Act (PPACA) mandated that many evidence-based preventive services be covered without cost sharing.11 Indeed, even before passage of the law, many CDHPs were offering primary preventive services without any charge to patients.
However, because PPACA only covers primary preventive care, some high-value treatments and services, especially those recommended in the treatment of common chronic diseases, may continue to be negatively incentivized under the CDHP. Plans can implement the next step in V-BID by targeting high-value secondary preventive services for which ample cost-benefit data exist. Increasingly, sophisticated information systems should tie together electronic medical records, clinical information (such as evidence-based guidelines), and financial data to create “personalized benefits” that optimize quality of care, encourage value and discourage waste.
A primary driver of the growth of CDHP products is the need for more affordable health care. However, without clinical nuance, the available evidence is clear that increases in beneficiary deductibles lead to meaningful decreases in the use many essential services. Incorporating V-BID principles will assist CDHP beneficiaries in making better decisions, creating a design that is both clinically effective and financially viable.
Clinical Nuance Infographic HDHP+ Infographic
References:
- Adapted from the 2007 article: Value-Based Insurance Design: A “Clinically Sensitive, Fiscally Responsible” Approach to Mitigate the Adverse Clinical Affects of High Deductible Consumer Directed Health Plans. Fendrick AM, Chernew ME. J Gen Intern Med. 2007;22(6):890-91. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2071958/
- American Association of Preferred Provider Organizations.
- Newhouse J, Insurance Experiment Group. Free for All? Lessons from the RAND Health Insurance Experiment. Cambridge, MA: Harvard University Press; 1993.
- Gibson TB, Ozminkowski RJ, Goetzel RZ. The effects of prescription drug cost sharing: a review of the evidence. Am J Manag Care. 2005;11:730–40. http://www.ncbi.nlm.nih.gov/pubmed/16268755
- Rice T, Matsuoka KY. The impact of cost-sharing on appropriate utilization and health status: a review of the literature on seniors. Med Care Res Rev. 2004;61(4):415–52. http://kff.org/medicare/the-impact-of-cost-sharing-on-appropriate/
- Heisler M, Langa KM, Eby EL, Fendrick AM, Kabeto MU, Piette JD. The health effects of restricting prescription medication use because of cost. Med Care. 2004;42:626–34. http://www.ncbi.nlm.nih.gov/pubmed/15213486
- Woolhandler S, Himmelstein D. Consumer directed healthcare: except for the healthy and wealthy it’s unwise. J Gen Intern Med. 2007. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2071952/
- Chernew ME, Gibson TB. Cost Sharing and HEDIS Performance. Medical Care Research and Review. 2008; 65(6):713-729. http://www.ncbi.nlm.nih.gov/pubmed/18559792
- Chernew ME, Shah MR, Wegh A, Rosenberg SN, Juster IA, Rosen AB, Sokol MC, Yu-Isenberg K, Fendrick AM. Impact Of Decreasing Copayments On Medication Adherence Within A Disease Management Environment. Health Affairs, 2008: 27; 103-112. http://content.healthaffairs.org/content/27/1/103.abstract
- Chernew ME, Juster IA, Shah M, Wegh A, Rosenberg S, Rosen AB, Sokol MC, Yu-Isenberg K, and Fendrick AM. Evidence That Value-Based Insurance Can Be Effective. Health Affairs, 2010: 29; 1-7. http://content.healthaffairs.org/content/29/3/530.abstract
- For a full list of covered services please see: http://www.uspreventiveservicestaskforce.org/Page/Name/uspstf-a-and-b-recommendations/