Patient-Centered Medical Homes and V-BID: A Highly Synergistic Approach to Achieve More Health for the Moneyi
Originally Produced: July 2012. Updated: July 2016
The past several decades have produced remarkable technological and therapeutic innovations in the prevention and treatment of disease resulting in impressive reductions in morbidity and mortality. These enhanced clinical outcomes coincide with a time of significant stress within our healthcare system – namely with the burden of costs of care. Although expenditure growth is the principle driving force behind health care reform, concerns remain regarding access to, and quality of, medical services. The challenge, therefore, is to enable continued improvements in care while containing expenditure growth. Unfortunately, few reform initiatives simultaneously address the issues of quality improvement and cost containment. As a result, “value” –the clinical benefit achieved for the money spent–is frequently excluded from the dialogue on how to manage spending.
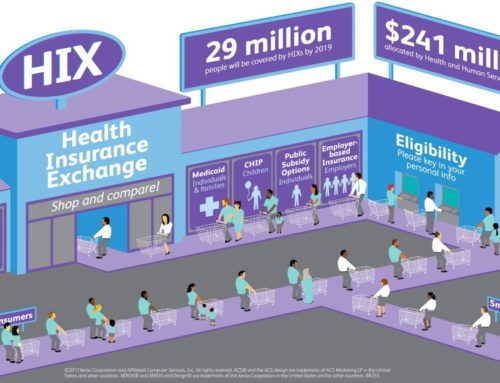
Currently popular payment reform initiatives such as global payments and accountable care organizations shift financial risks to health systems and clinicians. These cost-containment strategies infrequently address consumer behavior. The alignment of clinical and financial goals for providers and patients will likely mean faster achievement of system objectives of enhanced access, enhanced quality and slower cost growth. Patient Centered Medical Homes (PCMH) and Value-Based Insurance Design (V-BID) are two widely discussed innovations in health reform, yet the quality enhancing and cost containment potential of combining these ideas is rarely considered. Abandoning fee for service payment systems and cost-sharing strategies that raise prices for patients across the board, “clinically nuanced” reimbursements that provide strong quality incentives for providers, and benefit designs that incentivize beneficiaries to use high-value health services can improve health and productivity, and potentially lower long-run health care costs.
The PCMH model is a supply-side mechanism to enable clinicians to deliver better-quality care more efficiently. The PCMH model is not a quality improvement initiative per se, but rather a framework and platform that helps practices organize operaons and continuously improve care. The PCMH fosters relationships between patients and providers, improves access and incorporates office processes and payment systems to reward an ongoing physician-patient relationship and high-quality, coordinated care. Through better information management, use of guidelines and coordinated care, the PCMH may contribute to better quality, which in turn drives cost reductions through avoided hospitalizations and emergency department visits. Incentives are arranged so that doctors are compensated for the additional time and resources needed to intensively manage patient care.
V-BID seeks to enhance patients’ clinical outcomes and contain health care cost growth by changing demand-side (patient) incentives. The basic premise of V-BID is to remove barriers to essential, high-value health services. Using a “clinically nuanced” approach, patients assume an out-of -pocket cost proportional to the clinical value – rather than the price – of a given service. In doing so, V-BID incorporates available evidence regarding the clinical benefit (or lack thereof) for a given intervention, and can be tailored for application to a specific patient or group. By reducing barriers to high-value, evidence-based services and providers, V-BID plans can achieve improved patient-centered outcomes at any level of health care expenditure.
There is strong evidence that consumers respond to financial and non-financial incentives when it comes to health care choices. Studies show that when barriers to high-value care are reduced, patient compliance with recommended treatments increasesii and potential cost savings result.iii Conversely, raising the cost of medications that control chronic conditions can harm employees with chronic disease and increase costs for acute services like hospital visits.iv
Robust evidence also exists to support the PCMH approach to improving care quality. Individuals enrolled in medical homes are more likely to understand the plan for their care, have better self-management of symptoms, and have higher quality.v Patients who have a closer relationship with their primary care doctor also use more primary care services and take recommended medications more often.vi Medical homes can reduce gaps in care that breed wasteful redundancies, avoidable utilization, and lost productivity among employees. Studies have shown that information management systems used in medical homes can improve health care efficiency and effectiveness. To date, there are no published studies that examine the impact of combined VBID and PCMH.vii
By providing financial incentives like lower copayments for members who enroll in a PCMH, payers can use V-BID principles to influence provider choice. One innovative example of how V-BID can be used to encourage patients to receive care from high-performing provider is Blue Shield of California’s Blue Groove Plan, in which individuals with chronic diseases such as congestive heart failure, hypertension, and diabetes who select to receive their care from plan-specified high performing clinicians received enhanced benefits.
Delivery system improvement is relevant because even the best designed benefits cannot succeed at improving health outcomes unless the care delivered is evidence-based. Together, V-BID and PCMH can improve value by simultaneously making care more outcomes-driven, while reducing wasteful or unnecessary care.
Simply put, medical homes provide consumers with a more efficient means of getting care, while V-BID gives them incentives to make the switch to a new, more integrated system that will ultimately enhance patient-centered outcomes.
A wide spectrum of programs incorporating elements of both V-BID and PCMH in their health plans have been created. In-depth guides, including case studies, are available to employers and other interested individuals or groups.
Aligning Incentives and Systems: Promoting Synergy Between Value-Based Insurance Design and the Patient Centered Medical Home. Patient-Centered Primary Care Collaborative, 2010.
Value-Based Insurance Design Landscape Digest. Center for Value-Based Insurance Design, 2009.
Value-Based Benefit Design: A Purchaser Guide. National Business Coalition on Health, 2010.
References:
iBased on the whitepaper by AM Fendrick, B Sherman, D Whit. Aligning Incentives and Systems: Promoting Synergy Between Value-Based Insurance Design and the Patient Centered Medical Home. Patient-Centered Primary Care Collaborative, 2010. Accessed at: https://www.nbch.org/NBCH/files/ccLibraryFiles/Filename/000000000884/VBID-H2R-PCPCC%20v4-1101NBCH%20cover.pdf
iiChernew ME, Shah MR, Wegh A, Rosenberg SN, Juster IA, Rosen AB, Sokol MC, Yu-Isenberg K, Fendrick AM. Impact Of Decreasing Copayments On Medication Adherence Within A Disease Management Environment. Health Affairs, 2008: 27; 103-112. http://content.healthaffairs.org/content/27/1/103.long
iiiChernew ME, Juster IA, Shah M, Wegh A, Rosenberg S, Rosen AB, Sokol MC, Yu-Isenberg K, and Fendrick AM. Evidence That Value-Based Insurance Can Be Effective. Health Affairs, 2010: 29; 1-7. http://content.healthaffairs.org/content/29/3/530.full
ivHeisler M, Langa KM, Eby EL, Fendrick MA, Kabeto MU, Piette JD. The Health Effects of Restricting Prescription Medication Use Because of Cost. Medical Care. July 2004. 42(7):626-634. Accessed at: http://www.ncbi.nlm.nih.gov/pubmed/15213486
vRice T, Matsuoka KY. The impact of cost-sharing on appropriate utilization and health status: a review of the literature on seniors. Med Care Res Rev. 2004 Dec; 61(4):415-52. Accessed at: https://kaiserfamilyfoundation.files.wordpress.com/2013/01/the-impact-of-cost-sharing-on-appropriate-utilization-and-health-status-a-review-of-the-literature-on-seniors.pdf
viThe Commonwealth Fund. Closing the Divide: How the Medical Homes Promote Equity and Health Care: Results From the Commonwealth Fund 2006 Health Care Quality Survey. June 27, 2007 Volume 62. Accessed at: http://www.commonwealthfund.org/usr_doc/1035_Beal_closing_divide_medical_homes.pdf?section=4039
viiChaudhry B, Wang J, Wu S, Maglione M, Mojica W, Roth E, Morton SC, Shekelle PG. Systematic review: impact of health information technology on quality, efficiency, and costs of medical care. Ann Intern Med. 2006 May 16;144(10):742-52. Epub 2006 Apr 11. Accessed at: https://www.ncbi.nlm.nih.gov/pubmed/16702590