Originally Produced: August 2013 Updated: February 2014
V-BID in Action: Michigan Medicaid Expansion
Introduction
Value-Based Insurance Design (V-BID) is an innovative approach that can improve clinical outcomes and contain costs. The basic premise of V-BID is to align consumer incentives with value by reducing barriers to high-value health services and providers (“carrots”) and discouraging the use of low-value health services and providers (“sticks”). When “carrots” and “sticks” are used in a clinically nuanced manner, V-BID improves health care quality and controls spending growth. The concept of clinical nuance recognizes that: 1) medical services differ in the benefit provided; and 2) the clinical benefit derived from a specific service depends on the patient using it, as well as when and where the service is provided. By Incorporating greater clinical nuance into benefit design, payers, purchasers, taxpayers, and consumers can attain more health for every dollar spent.
Federal Government Allows V-BID in Medicaid
State Medicaid programs cover some of the nation’s most vulnerable citizens and account for a large and growing portion of state budgets. The Centers for Medicare and Medicaid Services (CMS) recently finalized rules (CMS-2334-F) giving state Medicaid programs greater flexibility to vary enrollee cost-sharing for drugs as well as certain outpatient, emergency department, and inpatient visits. If implemented successfully, a clinically nuanced cost-sharing model can enhance the use of high-value clinical services and reduce utilization of unnecessary and costly services, while fostering consumer engagement and personal accountability.
Cost-sharing for Outpatient and Inpatient Services: Under the new rule, Medicaid programs are permitted to impose cost-sharing (within certain income-based boundaries) on select outpatient services while allowing other services to be provided without cost sharing. Plans may also vary cost-sharing for a particular outpatient service in accordance with who provides the service and/or where the service is delivered. Further, the final rule allows state Medicaid agencies to target enrollee cost-sharing (within certain income-based boundaries) to specific groups of individuals based on clinical information
(e.g., diagnosis, clinical risk factors).
Non-emergent use of the Emergency Department: The new rule gives Medicaid plans the option to impose up to an $8 copayment for non-emergency services provided in the emergency department (ED).
Cost-sharing for Drugs: The rule provides states with the flexibility for differential cost-sharing on preferred ($0-$4) and non-preferred drugs (up to an $8 copay). The rule also retains the states’ ability to differentiate preferred and non-preferred drugs within their programs through
Preferred Drug Lists.
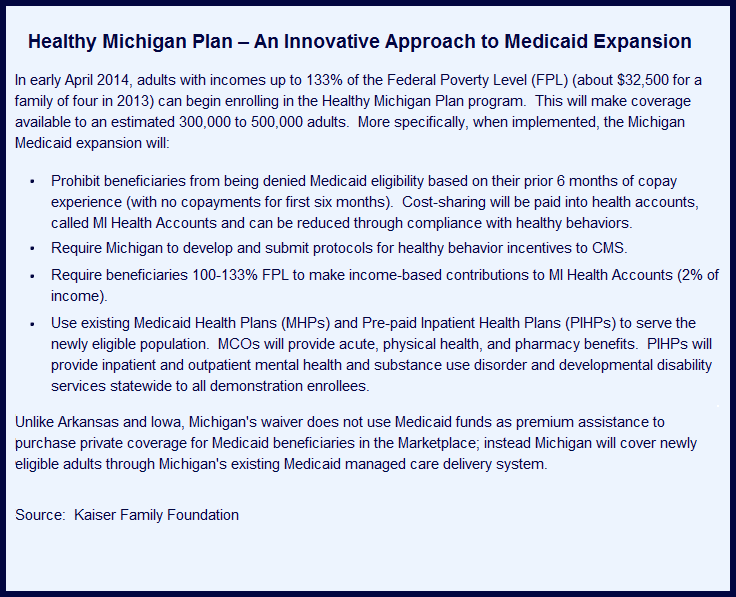
V-BID in Action: A Profile of “Healthy Michigan Plan” Medicaid
In September 2013, Michigan became the 25th state in the nation to expand Medicaid under the Affordable Care Act. The new Healthy Michigan Plan will provide coverage to an additional 470,000 residents over the next several years. Among the provisions of the Public Act 107 of 2013, the Healthy Michigan Plan relies on V-BID to improve access, control costs, and enhance personal responsibility.
Cost-sharing for Outpatient and Inpatient Services: Under Section 105D(1)(e), health plans are permitted to waive consumer copayments, “to promote greater access to services that the prevent the progression and complications related to chronic diseases.” Reducing barriers to evidence-based services across the continuum of care (e.g. visits, diagnostic tests, treatments) is the foundation of clinically nuanced benefit designs. Health plans may choose to exempt certain enrollees from cost-sharing for a specific service on the basis of a specific clinical indicator, while imposing cost-sharing on other enrollees for which the same service is not clinically indicated. For example, annual retinal eye examinations are recommended in evidence-based guidelines for enrollees with diabetes mellitus, but not recommended for those without the diagnosis.
Non-emergent use of the Emergency Department: Under Section 105D(1)(f), the Michigan Department of Community Health (MDCH) has been assigned to “design and implement a copay structure that encourages the use of high-value services, while discouraging low-value services such as non-urgent Emergency Department utilization.” To encourage high-value care, health plans might eliminate cost-sharing for office visits that take place at a recognized Patient-Centered Medical Home (PCMH), while imposing a copayment for clinician office visits outside a PCMH. To discourage low-value care, the Healthy Michigan Plan may choose to impose the maximum allowable cost-sharing for use of low value services—such as those identified in the Choosing Wisely initiative or the U.S. Preventive Services Task Force (USPSTF) Grade D recommendations. Unlike other services such as clinician visits and prescription drugs, the evidence-based application of “clinical nuance” is less clear in the emergency room setting. CMS, in partnership with the states, should ensure that increases in ED cost-sharing can be accurately applied only in truly non-emergent cases so that increased copayments for ED visits do not lead Medicaid enrollees to delay or forgo necessary care.
Cost-sharing for Prescription Drugs: Under Section 105D(5), the MDCH has been assigned to, “implement a pharmaceutical benefit that utilizes copays at appropriate levels allowable by CMS to encourage the use of high-value, low cost prescriptions.” This flexibility will allow Michigan to develop innovative cost-sharing structures that will encourage the use of high-value therapies and discourage harmful and low-value treatments. Under this model, preferred and non-preferred categories are determined based on their clinical value, not solely on their acquisition cost.
Conclusion
Incorporating V-BID into the Healthy Michigan Plan follows the recent CMS rule giving Medicaid programs greater flexibility to vary enrollee cost-sharing for drugs as well as certain outpatient, emergency department, and inpatient visits. When V-BID principles are used to set enrollee cost-sharing levels, Medicaid programs can improve quality of care, remove waste, foster consumer engagement, and mitigate the legitimate concern that non-nuanced cost-sharing may lead individuals to forgo clinically important care.