Originally Produced: May 2013 Updated: August 2015
The State Innovation Models Initiative: Using Clinical Nuance to Align Payer and Consumer Incentives
A video overview and SIM infographic accompany this issue brief.
Introduction
When the Center for Medicaid and Medicare Innovation announced the State Innovation Models (SIM) Initiative in 2012, state health planners and policymakers responded to the news with great enthusiasm. The SIM program was designed with unusually broad parameters to encourage innovation  in the development of new payment and delivery system models that improve health and promote efficiency. In addition, the program requires that reform strategies be coordinated across multiple plans and payers to stimulate collaboration. To aid in these measures, the SIM grants offer up to $60 million per state to support planning, testing, and model design.
in the development of new payment and delivery system models that improve health and promote efficiency. In addition, the program requires that reform strategies be coordinated across multiple plans and payers to stimulate collaboration. To aid in these measures, the SIM grants offer up to $60 million per state to support planning, testing, and model design.
Many states receiving SIM funding are planning to develop payment reform projects that restructure incentives for health care providers. Global budgets, pay-for-performance, bundled payment, and accountable care arrangements are examples of proposed approaches. However, promising “supply side” initiatives of this sort have historically paid little attention to consumer decision-making or the “demand side” of care-seeking behavior. Incentives for consumers can encourage the use of high-value care and providers and discourage the use of low-value care and providers. By aligning providers’ incentives with those for consumers, SIM projects can serve as a catalyst for these essential synergies and achieve impact beyond the sum of the parts.
 In reforming consumer incentives, grantee states can draw on the principles of Value-Based Insurance Design (V-BID). V-BID embodies the concept of clinical nuance, which recognizes that (1) medical services differ in the benefit provided, and (2) the clinical benefit derived from a specific service depends on the patient using it, as well as when, where and by whom the service is provided. Accordingly, V-BID plans reduce financial barriers to evidence-based services and high-performing providers (carrots) and/or impose disincentives to discourage use of low value services and provider (sticks). Several of the multi-million dollar SIM grants were awarded to states that explicitly included V-BID in their proposals as a mechanism to achieve more health for every dollar spent. These states include: Arkansas, Maine, Oregon, New York, and Connecticut.
In reforming consumer incentives, grantee states can draw on the principles of Value-Based Insurance Design (V-BID). V-BID embodies the concept of clinical nuance, which recognizes that (1) medical services differ in the benefit provided, and (2) the clinical benefit derived from a specific service depends on the patient using it, as well as when, where and by whom the service is provided. Accordingly, V-BID plans reduce financial barriers to evidence-based services and high-performing providers (carrots) and/or impose disincentives to discourage use of low value services and provider (sticks). Several of the multi-million dollar SIM grants were awarded to states that explicitly included V-BID in their proposals as a mechanism to achieve more health for every dollar spent. These states include: Arkansas, Maine, Oregon, New York, and Connecticut.
This extended issue brief and video overview highlight the merits of coordinating more efficient payment policies with clinically nuanced benefit designs, offer a roadmap for multi-payer implementation of these aligned strategies, and discuss possible uses for SIM funds to advance multi-payer V-BID implementation.
The Case for Multi-Payer Reform
Implementing innovative reimbursement policies and benefit designs consistently across payers can expedite the impact on clinical and economic outcomes beyond what a single payer could achieve. Multi-payer reform offers several advantages including:
Achieving critical mass for providers. Consider a clinician who routinely sees patients covered by Medicaid, traditional Medicare, Medicare Advantage plans, the state employee health plan, and a myriad of commercial health plans—each with their own approach to quality improvement and measurement, provider reimbursement, and benefit design. This clinician may not have the available time to learn the intricacies of each payer’s system, and ultimately decline to fully engage with certain programs. Coordinated multi-payer reform changes the equation so that clinicians can more easily accept new patients with streamlined payment options.
Overcoming a collective action problem. The average American will obtain coverage through several different payers over the course of his or her life. This means that any savings resulting from one payer’s investments in better care may partially or entirely benefit tomorrow’s payer. Given the upfront costs and time horizons that may be necessary to realize efficiencies in care, it may not be realistic for all payers and purchasers to adequately invest in valuable initiatives such as chronic management programs and prevention on their own. Universal multi-payer reform ensures that all payers contribute to the system in order to reap the benefits of insuring a more healthy population.
Achieving economies of scale. Coordinating payment policies across multiple payers will likely lead to a quicker, more efficient adoption rate of evidence-based policies. For example, in partnership with the American Academy of Family Physicians and the American College of Obstetricians and Gynecologists, the Choosing Wisely initiative strongly discourages scheduling elective, non-medically indicated inductions of labor or Cesarean deliveries before 39 weeks gestational age. If multiple payers collaboratively decide to stop paying for these potentially harmful practices, it is highly likely that providers will adhere to this higher level of patient care. The economies of scale of multiple payers collaboratively implementing evidence-based payment policies will increase adoption of such policies, leading to better care and lower cost.
A Roadmap for Multi-Payer Consumer and Provider Incentive Reform Implementation
Successful multi-payer reform implementation is complex and requires several elements including broad stakeholder buy-in and program customization. The following pages offer a roadmap that states can take to efficiently pursue multi-payer reforms that increase quality and decrease cost.
- Convene stakeholders to identify priorities and goals for health system reforms. Purchasers, payers, policymakers, providers, experts and consumers should come together to identify critical aims for reform. Priorities for consideration include the potential for improved health and avoidance of wasteful spending, alignment with local priorities, and the feasibility of combining programs with concurrent efforts. Throughout this process, data, evidence and experience should guide discussions to the maximum extent possible. Leadership from the state may be valuable for bringing together credible, high-level decision makers. State involvement can also assuage the anti-trust concerns that arise when competing payers collaborate.
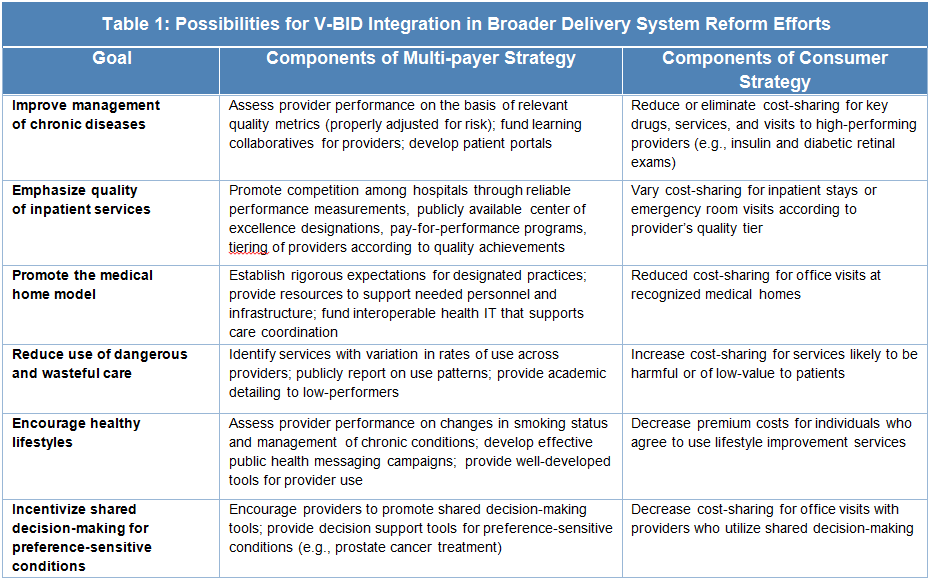
- Align incentives whenever possible while determine advantages and challenges for provider reform. The most successful models for reform will align both supply and demand side initiatives. Table 1 provides examples of synergistic multi-level approaches:
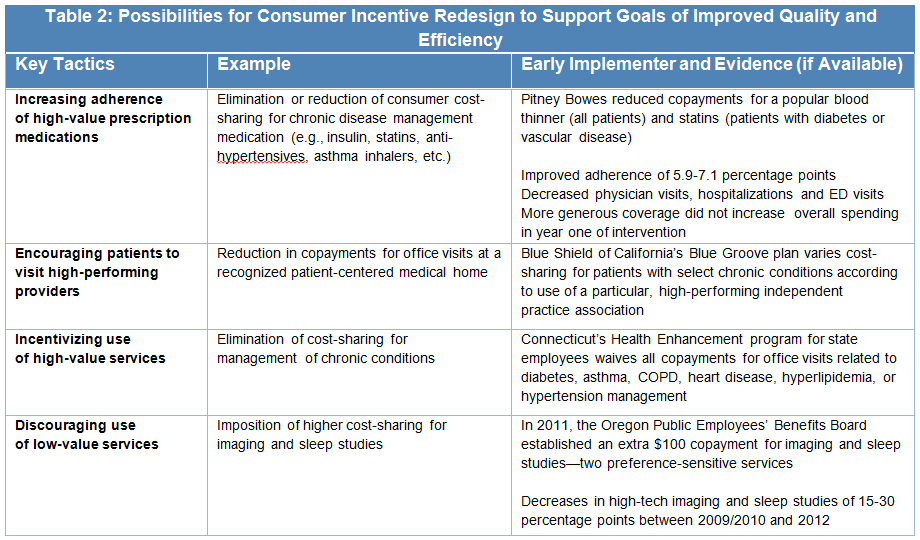
- Agree on when, where and for whom incentives and disincentives should be implemented: Once clinical scenarios requiring intervention are identified, stakeholders should explore, analyze, and reach consensus on the most relevant course of action. This includes taking into account all clinician and/or consumer decisions that affect outcomes for each targeted condition or behavior. Stakeholders can then consider options for carefully redesigning incentives—such as provider bonuses and out-of-pocket cost-sharing—to enable and encourage smart decisions. Stakeholders must also determine which clinicians and providers will be subject to the new incentives. For example, stakeholders may wish to waive copayments only for specific patient populations for which certain services are demonstrated to be highly effective. The experiences of early adopters highlighted in Table 2 may be instructive in considering options for consumer incentive redesign. (Additional examples and evidence may be found in this V-BID Center brief.)
- Agree on the extent of harmonization. Specific incentives—for instance, the amount of a clinician incentive or a patient copayment change —can be determined through a collaborative process or left to the discretion of individual plans. There is likely great value in aligning efforts around particular conditions, providers, and interventions, irrespective of whether or not the incentives and disincentives are exactly the same. Furthermore, complete harmonization may not be feasible or desirable given the particulars of the population being considered. This may be especially true for plans serving Medicaid enrollees, which are limited in their ability to impose disincentives.
- Design and encourage outreach efforts. Research indicates that consumers are inclined to accept innovative health care strategies, such as V-BID, especially when well-communicated. Best practices for consumer outreach include: ensuring transparency in the process of high and low-value designation; sharing stories to which patients can easily relate; and drawing on surveys to understand the population in question. Support and reinforcement from providers will be essential in a wide variety of these efforts. Even when the incentive is not directed at the clinician, there is still a key role to play. For example, clinician engagement can mean explaining to patients that essential medications can now be obtained with reduced out-of-pocket costs. Physicians should also be educated on any new disincentives to which their patients will be subject if they seek certain types of low-value care. Project leaders should cultivate physician champions and build relationships with state professional societies to spread awareness and to make sure that legitimate concerns are heard and addressed.
- Establish a timeline for implementation, evaluation, and appropriate follow-up. Ambitious but reasonable timetables for action can maintain momentum.
SIM funding is substantial, and it can support states as they explore, launch, or evolve V-BID implementation projects—especially those that are integrated with a broader strategy. Together, the SIM Round 1 and Round 2 awards have granted over $960 million to 35 states receiving some type of SIM award. A total of 17 states have already began work in implementing their SIM proposals, and 17 states receiving Round 2 Model Design Awards are set to submit their proposals within 12 months of receiving the award.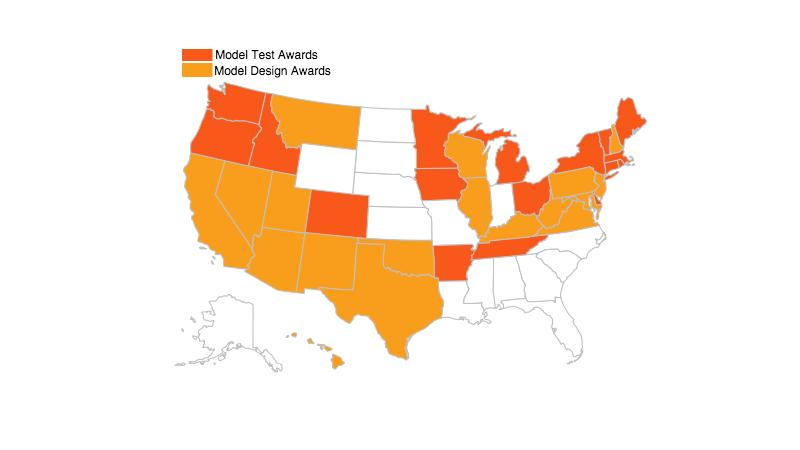
Conclusion
The broad parameters of the SIM Initiative provide tremendous flexibility to build more efficient, higher quality health care systems. Incorporating V-BID principles into payment reforms and consumer engagement initiatives can help states achieve that goal, especially when deployed consistently across multiple payers. The potential impact on quality improvement and cost containment is likely far greater than any single strategy could achieve.