
V-BID's Role in State Employee Health Plans
Over 19 million state and local employees, or about 10 percent of the total U.S. workforce, received health care through a public employee health plan in 2013. Facing growing health care cost burden, some state and local governments have turned to Value-Based Insurance Design (V-BID) as a way to decrease health costs, improve health, and maintain competitive benefit plans for employees.
V-BID alters the amount of consumer cost-sharing based on the health benefit provided by a specific clinical service — not the price. By aligning patients’ out-of-pocket costs with the value of services, V-BID can keep public employees healthier, reduce the number of sick days used, and improve workplace productivity.
In 2013, states paid $25.1 billion a year to provide benefits to their employees. Finding a way to control these costs effectively has become a priority for many state governors and legislatures. Additionally, across the U.S., an excise tax — sometimes referred to as a “cadillac tax” — for generous health plans goes into effect in 2020, and incentivizes employers to keep the benefit value of their individual health plans below $10,200, and their family health plans below $27,500.
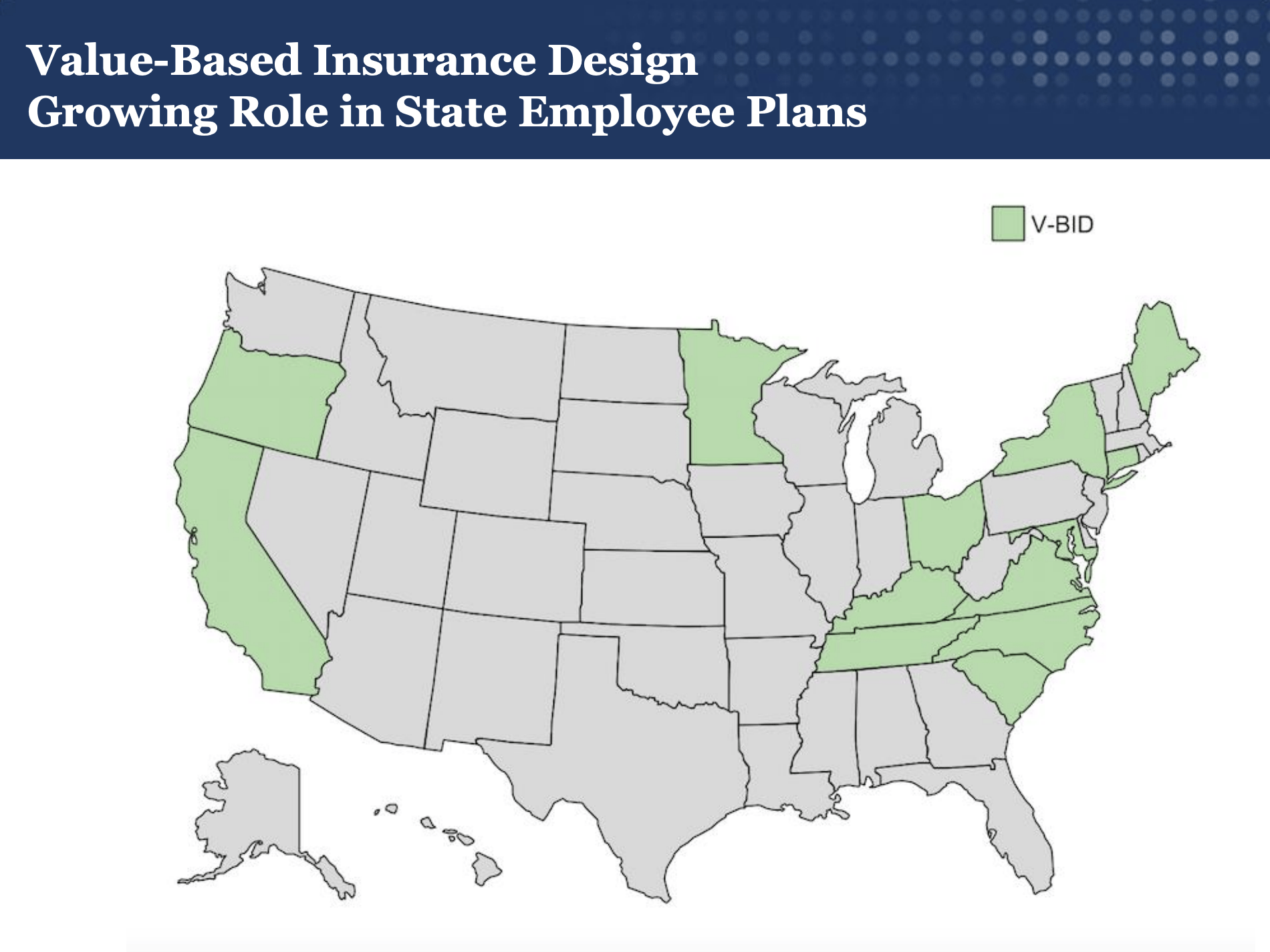
Multiple state and local governments have introduced value-based insurance design (V-BID) into their public employee benefit package to promote high value care and encourage employees to take an active role in managing their health care decisions. Most recently, Minnesota announced a pilot program, set to begin in 2018, that is based on V-BID principles and targeted toward state employees with diabetes.
In addition to discounts on their diabetes medications, eligible members will receive discounts on high-value medications that serve to comprehensively manage diabetes, like medication for high blood pressure, high cholesterol, and depression. When seeking to improve health outcomes and contain costs, the State of Connecticut implemented the Health Enhancement Program (HEP). The HEP incorporates clinically nuanced elements of V-BID into health plans for voluntarily enrolled state employees.
Connecticut's Health Enhancement Program
HEP incorporates clinically-nuanced elements of V-BID, eliminating barriers to evidence-based clinical services based on enrollee demographics and medical history
Prior to 2012, Connecticut’s state employee health plan did not distinguish between high-value services and low-value services in determining cost-sharing for beneficiaries. The HEP is different from other current plans because rather than uniformly increasing out-of-pocket costs, it lowers cost-sharing for recommended preventive care as well as services for five common chronic diseases. This program rewards enrollees for committing to responsibilities such as chronic disease management and evidence-based preventive care. Enrollees pay lower premiums and out-of-pocket costs compared to those who did not participate. Approximately 98% of eligible beneficiaries chose to enroll in the program.
During the first two years of the HEP, there was an increase in the use of targeted services and medication adherence for chronic conditions, as well as a decrease in emergency department use. As demonstrated in Connecticut, the added component of participation requirements to V-BID principles can help increase the utilization of targeted services. Early demonstration of increased use of services provides promising implications for long-term health and health care spending. As public and private payers are increasingly moving from volume-driven to value-based delivery systems, V-BID will continue to be an essential component. In light of the success of V-BID in Connecticut, there is every reason to suspect that HEP-like approaches will produce dividends in terms of health, satisfaction, productivity, and affordability.
