
In December 2024, the Centers for Medicare and Medicaid Services (CMS) announced that it will end the Medicare Advantage Value-Based Insurance Design (VBID) model in 2025 due to unsustainable costs driven by increased risk scores and Part D expenditures.
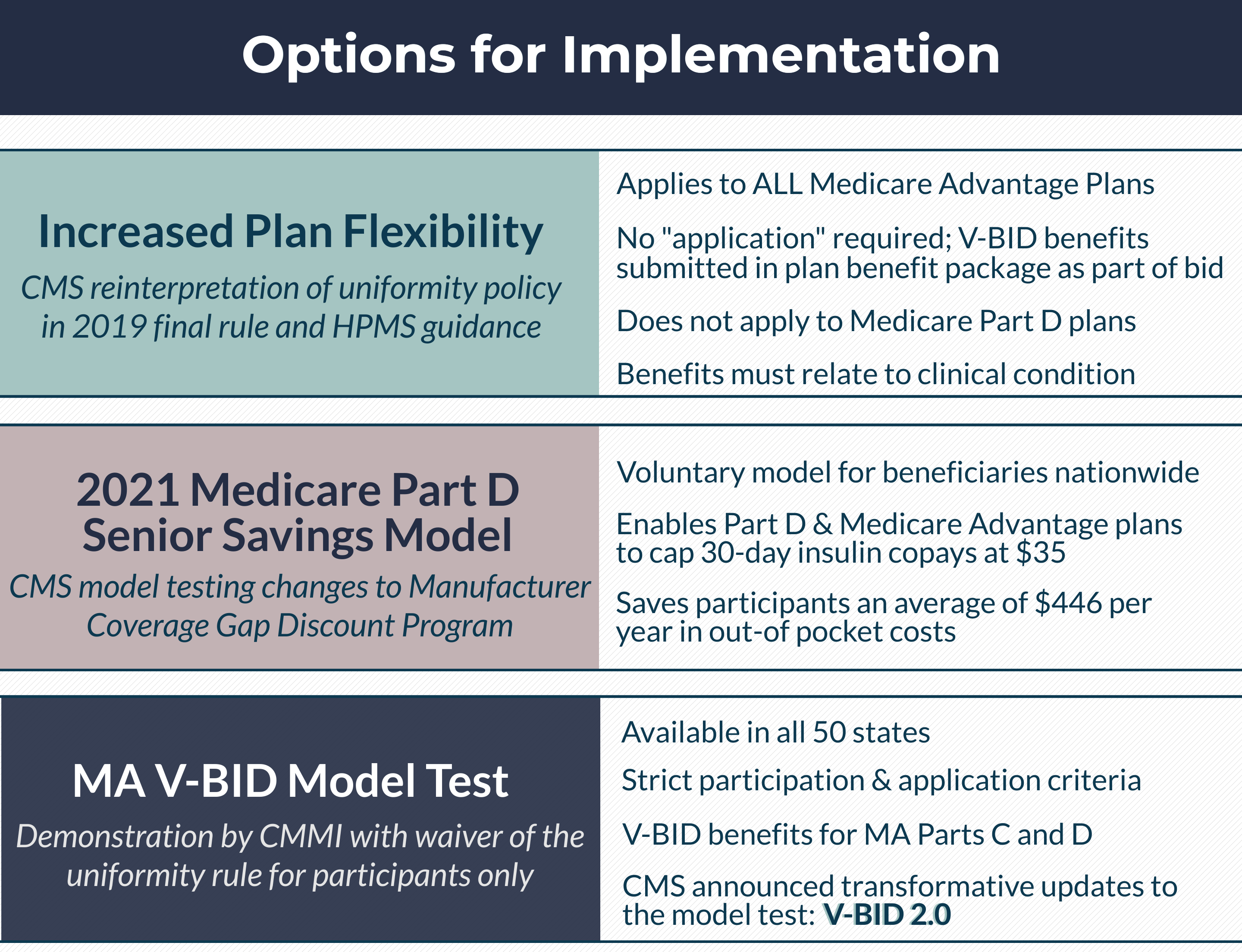
Lowering health care expenditures and ensuring access to high quality medical care for Medicare beneficiaries is a health policy priority. Value-Based Insurance Design (V-BID) is an innovative approach to consumer cost-sharing that can improve quality of care and potentially lower costs in the Medicare Program. V-BID plans are designed with the tenants of clinical nuance, recognizing that the clinical benefit derived from a specific service depends on the consumer using it, as well as when, where and by whom the service is provided. The most significant opportunity for V-BID implementation lies in the Medicare Advantage (MA) program. There are three options for incorporating V-BID principles in MA:
- The MA V-BID Model Test
- Increased plan flexibility allowed by the reinterpretation of the uniformity rule
- The Medicare Part D Senior Savings Model

On December 16, 2024, the Center for Medicare and Medicaid Services (CMS) announced that it will end the Medicare Advantage Value-Based Insurance Design (VBID) model in 2025 due to unsustainable costs of $4.5 billion over 2021 and 2022, driven by increased risk scores and Part D expenditures. While the model allowed MA plans to offer supplemental benefits, its termination is not expected to significantly impact MA plans since similar benefits are now widely available. To address cost-sharing concerns, CMS plans to introduce a voluntary $2 monthly cap on out-of-pocket drug costs starting in 2027.
History of the MA V-BID Model
On January 1st, 2017, the Center for Medicare and Medicaid Services (CMS) launched the Medicare Advantage Value-Based Insurance Design (MA V-BID) Model Test to assess the utility of structuring consumer cost-sharing and plan elements to encourage the use of high-value clinical services and providers. Nine MA plans in three of the seven eligible states (i.e. Massachusetts, Indiana, and Pennsylvania) were selected to enroll beneficiaries with specified chronic conditions in January 2017. In early 2018, the model test expanded to three additional states and included two additional clinical conditions. CMS later announced that, beginning in 2019, the V-BID model would include an additional fifteen new states (for a total of 25), allow Chronic Condition Special Needs Plans to participate, and allow participants to propose their own systems or methods for identifying eligible enrollees.
Pursuant to the Bipartisan Budget Act of 2018, in January 2019 the Centers for Medicare and Medicaid Services (CMS) released major changes to the current Medicare Advantage Value-Based Insurance Design (MA V-BID) model. From 2020 through 2024, these updates intended to lower costs, while increasing the quality and coverage of care for Medicare beneficiaries. The updated model, coined “V-BID 2.0”, broadened the scope of the existing Model by testing a wide range of MA service delivery and/or payment approaches including:
- Allowing customization of cost-sharing based on chronic condition, socioeconomic status, or both, including some non-health related benefits, such as transportation
- Expanding eligibility to include Chronic Condition SNPs, Dual Eligible SNPs, Institutional SNPs and Regional PPOs
- Bolstering the rewards and incentives programs that plans can offer beneficiaries to take steps to improving their health
- Increasing access to telehealth services
Additionally, CMS allowed for testing of the inclusion of Medicare’s hospice benefits into MA beginning in 2021. Special Needs Plans and Regional PPOs in all states and territories are now eligible to apply. Through increased testing of clinically-nuanced strategies in MA plan benefit designs, the MA V-BID Model evaluated the effectiveness of aligning out-of-pocket costs with the clinical value of services, with the goals of improving health outcomes and lowering expenditures for Medicare Advantage enrollees. Although CMS announced the VBID model’s termination in 2025 due to high costs, its lessons will shape future benefit designs, though challenges remain in sustaining cost-sharing waivers for low-income members.

On April 16th, 2018, CMS officially published their new rule for the Medicare program contract year 2019. This rule includes a reinterpretation of the Medicare Advantage (MA) uniformity requirement that will allow for more flexibility in benefit design for MA enrollees with specified chronic conditions.
Beginning in 2020, CMS will waive the uniformity requirement for MA plans that provide additional supplemental benefits to chronically ill enrollees. This change paves the way for the further incorporation of V-BID principles into the Medicare Advantage program. While the ongoing MA V-BID Model Test will continue, plans outside of the demo will now have the flexibility to offer V-BID benefit designs to their beneficiaries without being subject to the additional application and geographic limitations inherent to the model test. Although the ability to lower cost-sharing for prescription drugs will remain a unique feature of the MA V-BID demo, the application of clinically nuanced V-BID strategies beyond the model test presents an enormous opportunity for the Medicare Advantage program. V-BID can encourage the utilization of high-value providers and services, thus helping Medicare Advantage plans improve health and quality, enhance consumer engagement, and reduce costs.
On March 11th, 2020, CMS announced the new 2021 Medicare Part D Senior Savings Model. The new model may dramatically reduce the out-of-pocket cost of insulin for over 3 million of its Medicare beneficiaries.
Beginning on January 1st, 2021, CMS will test a change to the Manufacturer Coverage Gap Discount Program to allow Medicare Part D and Medicare Advantage sponsors nationwide to offer a benefit design that includes predictable co-pays for insulin. Beneficiaries who opt-in to this voluntary model will be able to receive a thirty-day supply of a broad set of plan-formulary insulins for no more than $35. Participating beneficiaries are expected to save an average of $446 per year in out-of-pocket costs relative to average cost-sharing amounts in 2020. This implementation of V-BID principles has the potential to help millions of diabetic Medicare beneficiaries access insulin and manage their diabetes by reducing financial barriers to care and stabilizing monthly costs.
V-BID White Paper:
Incorporating Value-Based Insurance Design to Improve Chronic Disease Management in the Medicare Advantage Program
The V-BID Center White Paper, “Incorporating Value-Based Insurance Design to Improve Chronic Disease Management in the Medicare Advantage Program,” concludes that V-BID programs which reduce consumer cost-sharing for high-value services and providers are a fiscally feasible option for the Medicare program. A review of the peer-reviewed literature reveals how increases in Medicare beneficiary cost-sharing are adversely affecting our most vulnerable beneficiaries, contributing to poor patient-centered outcomes, and, in some instances, increasing Medicare expenditures. Actuarial modeling of MA V-BID programs for diabetes mellitus (DM), chronic obstructive pulmonary disease (COPD), and congestive heart failure (CHF) demonstrates that consumer out-of-pocket costs are reduced in all 3 conditions, plan costs increase slightly in the short term for certain conditions (DM and COPD), and plan savings result for CHF. From the societal perspective, the DM program was close to cost neutral; net savings resulted in the COPD and CHF programs.
Applying clinically nuanced V-BID strategies presents an enormous opportunity for the Medicare program – particularly Medicare Advantage plans. V-BID can encourage the utilization of high-value providers and services and limit the use of services that are of potentially low-value, thus helping Medicare Advantage plans improve health and quality, enhance consumer engagement, and reduce costs.
For more information, please view the resources below:
