Implementing V-BID in State Medicaid Plans
State Medicaid programs cover some of the nation’s most vulnerable citizens and account for a large and growing portion of state budgets. In 2013, the Centers for Medicare and Medicaid Services (CMS) finalized rules (CMS-2334-F) giving state Medicaid programs greater flexibility to vary enrollee cost-sharing for drugs as well as certain outpatient, emergency department, and inpatient visits.
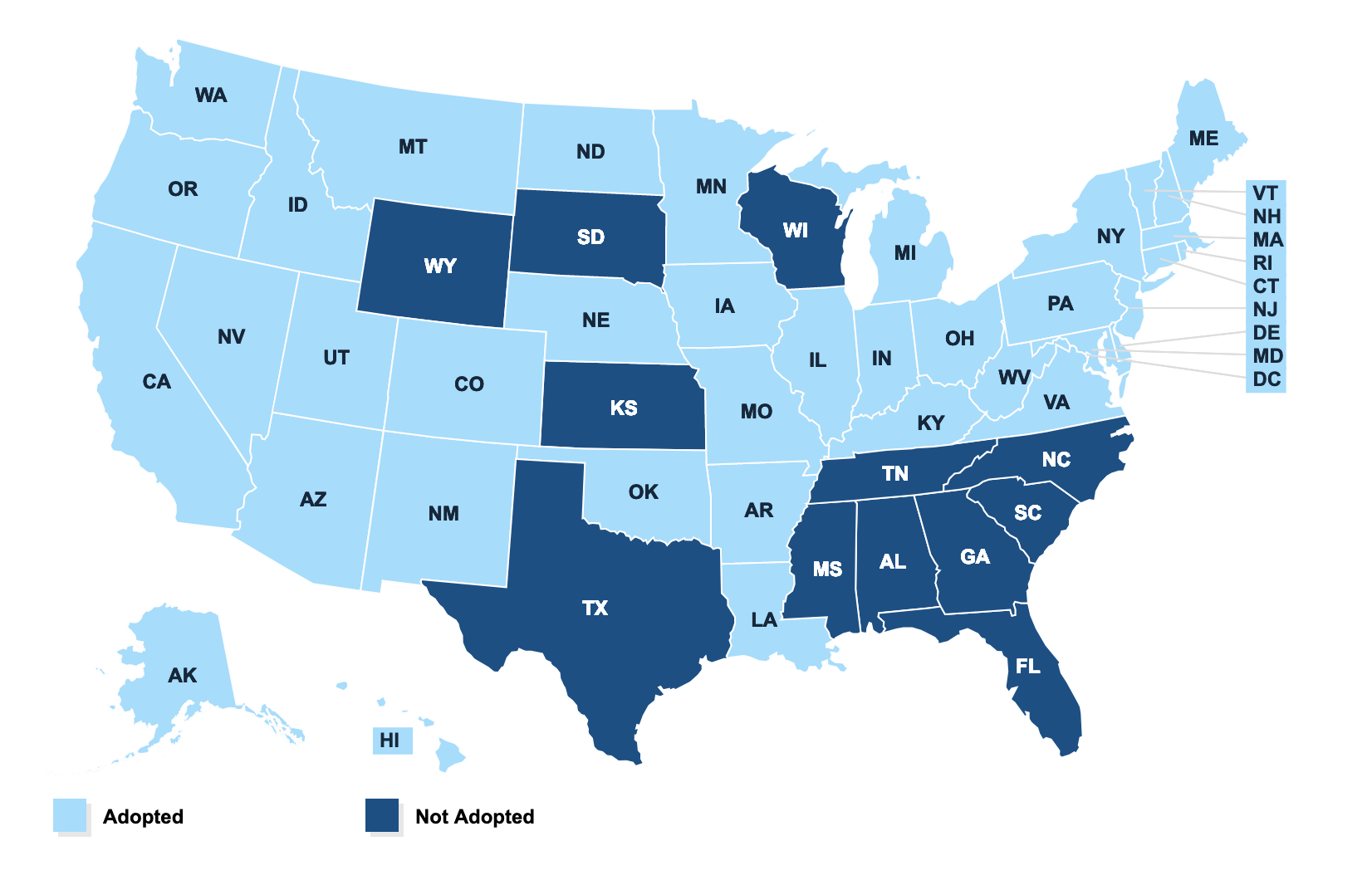
Under the Affordable Care Act (ACA), states have the option of expanding Medicaid eligibility with the financial support of the federal government. As Medicaid enrollment expands, some states have embraced this as a prime opportunity to take advantage of these new flexibilities to design value-based plans (V-BID) that engage beneficiaries and improve health outcomes.
If implemented successfully, a clinically nuanced cost-sharing model can enhance the use of high-value clinical services and reduce utilization of unnecessary and costly services, while fostering consumer engagement and personal accountability. Using V-BID principles to set enrollee cost-sharing levels, Medicaid programs can improve quality of care, remove waste, and mitigate the legitimate concern that non-nuanced cost-sharing may lead individuals to forgo clinically important care.
August 17, 2020