Low-value care can be defined as “[s]ervices that provide little or no benefit to patients, have potential to cause harm, incur unnecessary cost to patients, or waste limited healthcare resources,” and contributes to over $345 billion annually in wasteful health spending.
Addressing Low-Value Care
The United States spends more, both per capita and as a percent of GDP, on health care than any other country, yet fails to achieve commensurate health outcomes. One reason for this discrepancy between health spending and outcomes is the significant amount – upwards of $340 billion per year – that the U.S. spends on low-value care.
Driven by human bias, information disparities, provider’s litigation concerns, and fee-for-service payment systems, low-value services provide no additional health benefit and, in some instances, may even be harmful to patients. Instances of low-value care can also lead to costly cascades of additional, unnecessary care. With a pressing need to reduce costs and improve quality within the U.S. health care system, reducing the use of low-value services should be a priority for providers, purchasers, and patients. The identification and removal of low-value care would result in immediate and substantial savings to create headroom for increased expenditures on high-value services.
Current Efforts
Value-based insurance design improves health care quality and efficiency by reducing cost sharing for services that have strong evidence of clinical benefit. The same goals can also be accomplished by decreasing cost sharing for high-value services while increasing cost sharing for low-value services, ensuring more effective care and achieving net cost savings.
However, there are challenges in defining what is meant by “low-value services” and implementing programs to restrict such services’ use. Investments in processes to define low-value care, comparative effectiveness research to identify services that produce harm or marginal clinical benefit, and information technology to implement findings can facilitate applying value-based insurance design to the low-value realm that result in immediate and substantial savings.
In going beyond identification, this new initiative has the potential to catalyze meaningful change in the treatment of low-value care and has garnered well-deserved support and attention – as showcased by recent articles in Health Affairs and The New York Times. It’s time to take action against the financial and health burden of low-value care. Previous efforts to identify, measure, and reduce the use of low-value clinical services have been met with challenges. The V-BID Center has developed four steps to address low-value care: identify, measure, report, and reduce.

Identify
Campaigns such as the Choosing Wisely initiative have called upon health care providers to identify low-value services, but without corresponding action by purchasers and other stakeholders, progress has been slow. Building upon the lessons of the Choosing Wisely initiative, the Task Force on Low-Value Care has identified a “Top-Five” list of low-value clinical services for purchasers to target for reduction. The selected services were chosen based on their association with harm, their cost, their prevalence, and the availability of concrete methods to reduce their use. The “Top-Five” include:
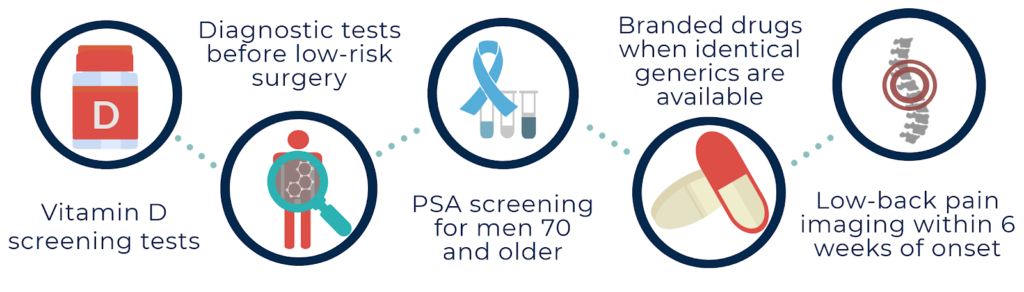
These services—chosen with the tenants of clinical nuance in mind—offer little to no clinical value, expose patients to unnecessary harm, and collectively contribute to over $25 billion annually in wasteful health spending. Additionally, the U.S. Preventive Services Task Force (USPSTF) identifies certain medical services as being “D-Rated,” meaning that “there is moderate or high certainty that the service has no net benefit or that the harms outweigh the benefits.”
Measure
All-Payer Claims Databases (APCD) are state-run collections of health insurance claims from both public and private payers and provide valuable information for quantifying the prevalence of low-value care in individual states. Currently, 20 states have enacted some form of an APCD. In addition, the MedInsight Waste Calculator, an analytical tool developed by V-BID Health and Milliman, can compute the cost of wasteful care in the health care system. The Medicare Payment Advisory Commission (MedPac) also assembles claims data on low-value care, specifically within Medicare, defining low-value care with recommendations made by the Choosing Wisely Campaign and USPSTF.
Report
States are uniquely situated to report instances of low-value care, as APCD are state-run. In 2014, The Commonwealth of Virginia reported spending $586 million on unnecessary costs using data from their APCD. In this analysis, the state found more was spent on low-cost, low-value services, than high-cost, low-value services. Analyzing and communicating this data creates an opportunity to target systematic patterns of waste.
Reduce
The culmination of this four-step process, reduction of low-value care utilization, can be achieved through the use of levers by various health care stakeholders. Levers can be both provider- and patient-facing, and are intended to discourage or encourage certain behaviors with the ultimate goal of reducing low-value care consumption.
Using the information gathered in the earlier three steps of this process, stakeholders will be able to identify levers to implement that best fit their situation. For example, Section 4105 of the Patient Protection and Affordable Care Act implements a provider-facing lever by amending the Social Security Act to remove Medicare payments for services identified as D-Rated by the USPSTF. In California, two medical centers implemented an intervention to reduce one of the “Top 5” low-value services, and an overall large source of low-value care: diagnostic testing and imaging for low-risk patients prior to low-risk surgery.
In light of findings from the claims data, the Virginia Center for Health Innovation (VCHI), in collaboration with the V-BID Center, launched a statewide pilot aimed at reducing the utilization of low-value care. This pilot is an excellent example of how stakeholders can implement the four-step process of Identify, Measure, Report and Reduce to achieve a wide-reaching goal to reduce costs and improve the quality of care by targeting low-value services.
Innovative Benefit Design to Reduce Low-Value Care
As Americans are being asked to pay more out-of-pocket for all services, regardless of clinical value, the V-BID Center is committed to enhancing access and affordability to high-value services. Lower consumer out-of-pocket costs would modestly increase utilization of essential clinical services. To pay for the incremental spending, a range of nuanced cost-reducing strategies should be pursued to create “headroom” for additional spending on high-value services. In a country that spends over $345 billion annually on low-value care, there is ample opportunity to attain cost savings without shifting costs to the consumer for clinically-indicated care.
V-BID X, a cost-neutral health plan incorporating value-based principles, implements the patient-facing lever of Value-Based Insurance Design to reduce the use of specific low-value services, enabling expanded coverage for high-value care. V-BID X plans demonstrate that coverage can lower consumer out-of-pocket costs for high-value services without increasing deductibles or premiums. Applying targeted cost-sharing based on the clinical value – not price – of a service will allow consumers improved access to high-value care, reduce cost-related non-adherence, and decrease exposure to harmful care.

