On Tuesday, December 12, 2017, the President signed the $700 billion National Defense Authorization Act for fiscal year 2018. The 2018 NDAA further incorporates V-BID principles into the TRICARE Pharmacy Benefits Program.
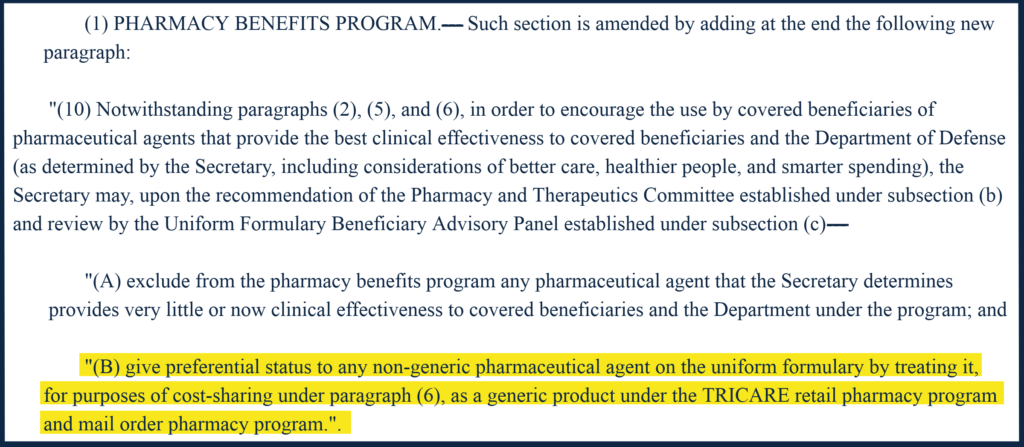
Section 702 (C) (b) (1) (B) modifies cost-sharing requirements to give preferential status to any non-generic pharmaceutical agent on the uniform formulary by treating it as a generic product under the TRICARE retail pharmacy program and mail order pharmacy program. This modification is consistent with the V-BID Center’s ‘precision benefit design’ concept.

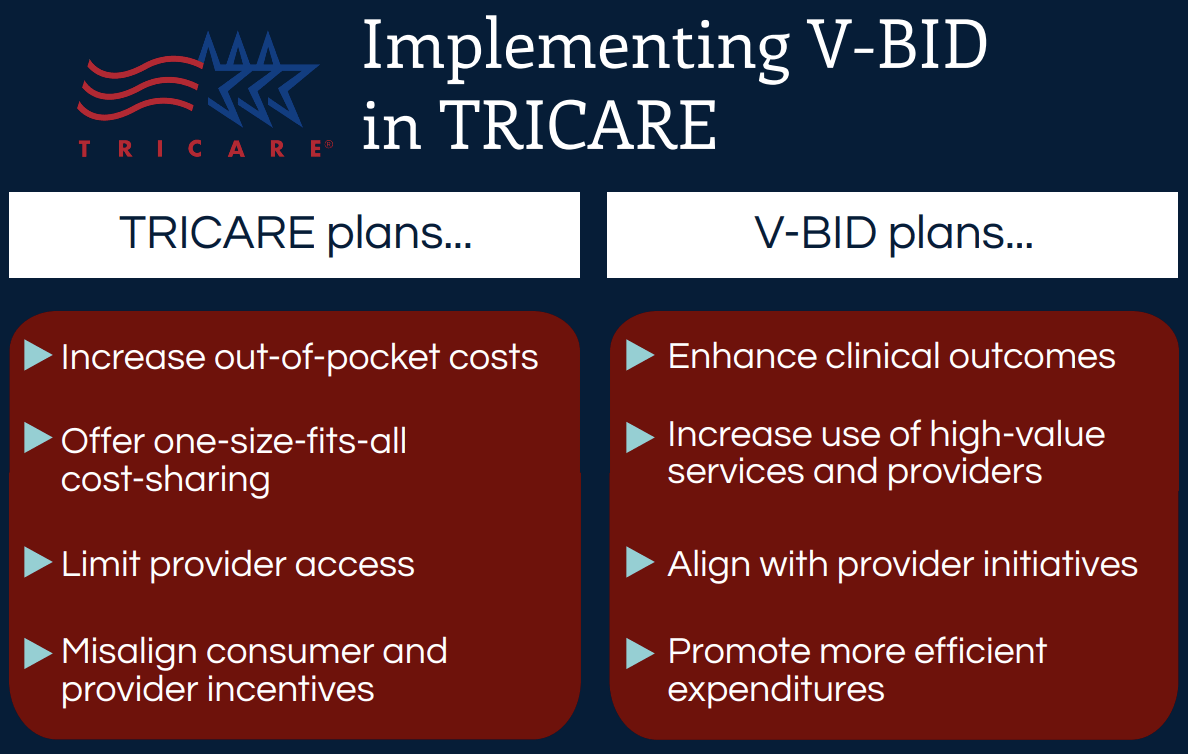
Access to quality care and containing costs are among the most pressing issues for our military personnel and our national well‐being and economic security. Moving from a volume‐driven to value‐based military health delivery system requires a change in both how we pay for care and how we engage consumers to seek care. However, less attention has been directed to how we can alter consumer behavior as a policy lever to bring about a more efficient delivery system.
In order to achieve our clinical and financial goals for military health care, value-driven consumer incentives — through benefit design reforms that promote smart decisions and enhanced responsibility — must be aligned with payment reform initiatives.
Evading the Dangers of a Blunt Approach to Beneficiary Cost-Sharing
With some notable exceptions, most U.S. health plans – including TRICARE – implement consumer cost-sharing in a ‘one-size-fits-all’ way, in that beneficiaries are charged the same amount for every doctor visit, diagnostic test, and prescription drug. As TRICARE members are asked to pay more for their medical care, a growing body of evidence demonstrates that increases in consumer cost-sharing lead to decreases in the use of both non-essential and essential care. Since there is evidence of both underuse of high-value services and overuse of low-value services in the TRICARE program, ‘smarter’ cost-sharing is a potential solution — one that encourages TRICARE members to use more of those services that make them healthier, and discourages the use of services that do not.
Unfortunately, research suggests that increasing 'skin in the game'
has not produced a savvier health care consumer.
Infusing ‘Clinical Nuance’ into TRICARE