

Insurers Test Re-Enacting Cost-Sharing for COVID-19 Treatment
Three of the nation’s Blue Cross and Blue Shield affiliates have re-enacted cost-sharing for COVID-19 treatment. While the CARES Act mandates insurers cover all medically necessary testing and vaccine costs, commercial insurers are not required to fully cover treatment costs. Insurers should implement a value-based benefit design for COVID-19 care and eliminate cost-sharing to prevent patients from not seeking out necessary treatment due to cost.

Out-of-Pocket Spending for Influenza Hospitalizations in Medicare Advantage
In an analysis of elderly Medicare Advantage patients, the mean out-of-pocket spending for influenza hospitalizations was almost $1,000. These findings indicate the potential magnitude of patient cost-sharing if cost-sharing waivers for COVID-19 hospitalizations are allowed to expire. Cost-sharing waivers should be swiftly, generously, and continually implemented to allow patients to receive necessary COVID-19 care.
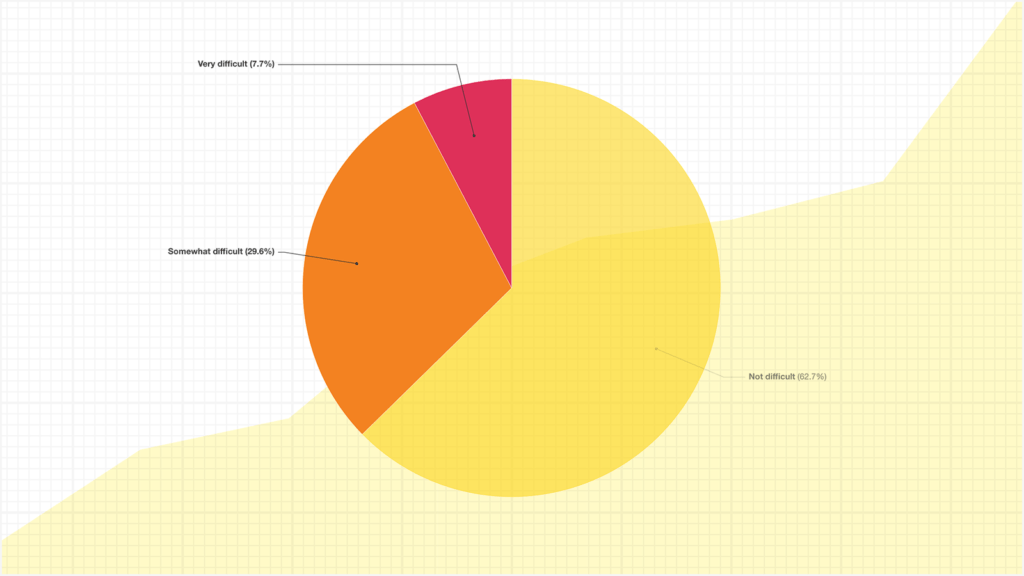
Survey: Americans Struggle to Afford Medications As COVID-19 Hits Savings and Insurance Coverage


How Does Cost-Sharing Impact Spending Growth and Cost-Effective Treatments? Evidence from Deductibles

High Out-of-Pocket Costs Lead to Financial Concerns, Lifestyle Changes for Seniors

Spending and Out-of-Pocket Prices for Brand-Name Drugs Among Commercially Insured Individuals in Massachusetts

The Impact of Social Determinants of Health on Medication Adherence: a Systematic Review and Meta-Analysis

Online Advertising Increased New Hampshire Residents' Use of Provider Price Tool But Not Use of Lower-Price Providers

A Few Hundred Dollars Makes a Difference in Use of Long-Lasting Birth Control
After the Affordable Care Act’s no-cost preventive services provision took effect, women in high-deductible health plans opted for long-acting reversible contraceptives more frequently than women in other health plans. Women who faced the highest costs before the ACA mandate increased their use of LARC methods the most following cost-sharing elimination, highlighting the impact out-of-pocket costs have on contraceptive choice.


"Incredibly Concerning" Lawsuit Threatens No-Charge Preventive Care for Millions
How Payers Can Identify, Reduce Low-Value Care Spending Patterns
Identifying and eliminating low-value care will be crucial to improving overall health care spending and patient outcomes. To meaningfully reduce low-value care spending, a concerted and deliberate effort among payers and other stakeholders will be needed. Learn more from this recent feature of the V-BID Center’s work on low-value care.
Survey Finds Majority of Employers Support Drug and Hospital Pricing Reform

Savvy Employers Alter Status Quo to Address Drugs, Deductibles and Disincentives for Treatment
In 2019, the IRS issued guidance allowing HDHPs with health savings accounts to cover an expanded list of preventive services and medications before patients meet their plan’s annual out-of-pocket deductible. In concordance with the guidance, one in five employers waived some cost-sharing for prescription drugs in 2020 to encourage employees with chronic illnesses to adhere to their treatment plan.


Recent Webinar: Virtual V-BID Summit 2021 - 20 Years of Impact & Innovation
Please Help Support the V-BID Center
As a non-profit entity, the V-BID Center relies on fundraising to support our research, education, and policy efforts. Please help us continue our work by donating here. We truly appreciate your consideration.


