The Evidence for V-BID: Validating an Intuitive Concept
Introduction
In November 2012, the National Coalition on Health Care recognized value-based insurance design, also referred to as V-BID, as a health system “game-changer.”i The Coalition affirmed the critical role of ‘clinical nuance’ in health benefit design and payment reform, acknowledging that 1) health services differ in the amount of clinical benefit provided, and 2) the clinical benefit derived from a specific service depends on the patient using it, as well as when, where, and by whom the service is provided. The basic V-BID premise is to align patients’ out-of-pocket costs, such as copayments and deductibles, with the value—not the cost—of health services.ii-iv Thus, the more beneficial the service, the lower the out-of-pocket cost. By reducing barriers to high-value services (through lower cost-sharing) and discouraging low-value services (through higher cost-sharing), V-BID plans can achieve better health outcomes at any level of health care expenditure.
Since the Coalition’s 2012 announcement, a variety of stakeholders and programs have recognized the potential for V-BID to improve value in health care, especially when deployed in alignment with other tactics. V-BID has been recommended by several major bipartisan health reform proposals, and is explicitly included in federal legislation, multiple state SIM initiatives, new federal Medicaid guidance, and state Medicaid legislation in Michigan.
Summary
The sample of peer-reviewed research summarized in this brief validates the intuitive logic of V-BID. The available literature indicates that incentive-based V-BID programs (“carrots”) can improve quality of care and reduce undesirable acute care utilization such as emergency room visits and hospitalizations. When targeted correctly, these incentive-only programs can be cost neutral in regard to direct medical expenditures over the medium term. A less extensive body of evidence indicates that higher cost-sharing on low-value services (“sticks”) can reduce wasteful spending and help moderate health care cost growth.
The Impact of Consumer Cost-Sharing on Cost and Quality
Suboptimal use of evidence-based health care services is well-documented. The literature indicates conclusively that increases in patient cost-sharing adversely impacts compliance with recommended high-value services across the entire continuum of clinical care.v-vii
This cost-related noncompliance is often associated with higher rates of hospitalization, morbidity, and mortality—and in certain instances, higher overall health costs—for patients with chronic disease. A 2007 synthesis of the impact of cost-sharing on pharmaceutical utilization concluded:
Increased cost-sharing is associated with lower rates of drug treatment, worse adherence among existing users, and more frequent discontinuation of therapy. For each 10% increase in cost-sharing, prescription drug spending decreases by 2% to 6%. . .For some chronic conditions, higher cost-sharing [/fusion_builder_column]
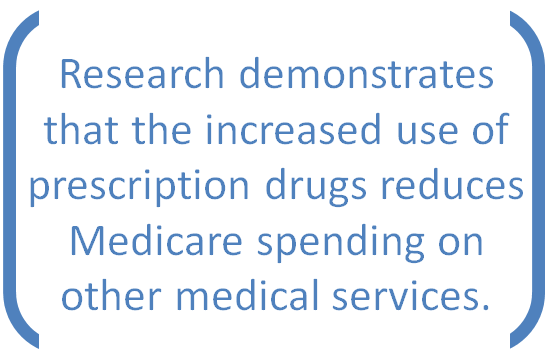 Conversely, as cost-sharing is lowered, higher rates of adherence result. These incentive-driven programs can pay for themselves by reducing hospitalizations and emergency department visits. Notably, in a November 2012 report, the Congressional Budget Office concluded—for the first time—that the available research demonstrates that the increased use of prescription drugs reduces Medicare spending on other medical services.viii
Conversely, as cost-sharing is lowered, higher rates of adherence result. These incentive-driven programs can pay for themselves by reducing hospitalizations and emergency department visits. Notably, in a November 2012 report, the Congressional Budget Office concluded—for the first time—that the available research demonstrates that the increased use of prescription drugs reduces Medicare spending on other medical services.viii
Table 1 presents a selection of peer-reviewed, well-controlled V-BID evaluations. Four studies assessing V-BID’s impact on resource use and cost concluded that the added expense attributed to the modest increases in targeted high-value services did not raise aggregate direct medical costs over the medium term; few reported net savings. Even those programs that are not cost-neutral can deliver impressive return on investment: a 2014 study of Blue Cross Blue Shield of North Carolina members found that an untargeted intervention could recover 89% of the sponsor costs for hypertensive patients.
Table 1: V-BID’s Impact on Cost, Quality and Health Status
Of the studies available, very few have accounted for improvements in productivity associated with better health. These non-medical economic effects are difficult to measure, but research suggests that their inclusion would have a significant positive impact on the financial consequences of V-BID programs.ix
It bears noting that not all V-BID implementations have equal impact. In a recent Health Affairs review of 76 V-BID plans, Choudhry and colleagues identified specific program attributes that are associated with greater success. V-BID programs that are more generous, limit eligibility to high-risk patients, offer wellness programs, and make the benefit available only for medication ordered by mail tend to have greater impact on adherence than plans without these features.x
Disincentive-Based Interventions
 A V-BID approach to low-value services avoids indiscriminate “across-the-board” increases in patient cost-sharing that can simultaneously reduce the utilization of high-value services.vi,vii, xxi,xxii Rather, V-BID uses clinically targeted increases in cost-sharing to discourage patients from using specific low-value services, such as those identified through the Choosing Wisely project.xxiii A V-BID program that includes both carrots and sticks may be particularly desirable for payers interested in implementing a plan that is cost-saving from an actuarial perspective in the short-term. While disincentive programs are less popular than those that offer positive incentives, qualitative research from focus groups suggests that consumers may be willing to accept disincentives provided processes for identifying low-value services are perceived as fair and transparent.xxiv-xxvi
A V-BID approach to low-value services avoids indiscriminate “across-the-board” increases in patient cost-sharing that can simultaneously reduce the utilization of high-value services.vi,vii, xxi,xxii Rather, V-BID uses clinically targeted increases in cost-sharing to discourage patients from using specific low-value services, such as those identified through the Choosing Wisely project.xxiii A V-BID program that includes both carrots and sticks may be particularly desirable for payers interested in implementing a plan that is cost-saving from an actuarial perspective in the short-term. While disincentive programs are less popular than those that offer positive incentives, qualitative research from focus groups suggests that consumers may be willing to accept disincentives provided processes for identifying low-value services are perceived as fair and transparent.xxiv-xxvi
A Note of Caution
A number of reasonable concerns have been raised regarding the methodologies used in acquiring the existing evidence on V-BID, as well as the reliability and applicability of that evidence. ii,iii,xxvii
Some of the most commonly raised limitations include:
- Plausibility of publication bias (i.e., the failure to publish unfavorable results)
- Use of total cost rather than plan sponsor cost
- Limited use of randomized controlled trials
- Potential for conclusions to be drawn from study populations that are not representative
- Methodological issues such as confounding interventions and incompletely reported data
Conclusion
V-BID implementations encompassing the entire continuum of clinical care are feasible options for payers, purchasers, and policymakers interested in achieving more health for every health care dollar spent. Despite the documented conceptual and methodological concerns, consistent patterns are emerging in the literature: incentive-based V-BID programs modestly increase utilization of targeted services, usually with no increase in direct medical expenditures. Inclusion of indirect economic benefits of improved health, such as disability reduction and improvements in productivity, will further enhance the return on investment.ix Further, when incentive-based V-BID programs are combined with targeted “stick” programs that reduce the use of harmful or unproven services, it is realistic to assert that clinically nuanced designs have potential to simultaneously improve quality and contain costs.
References
- National Coalition on Health Care. Curbing Costs, Improving Care: The Path to an Affordable Health Care Future [Internet]. [cited 2012 Nov 30]. Available from: http://www.nchc.org/plan-for-health-and-fiscal-policy/
- Fendrick AM, Smith DG, Chernew ME, Shah SN. A Benefit-Based Copay for Prescription Drugs: Patient Contribution Based on Total Benefits, Not Drug Acquisition Cost. American Journal of Managed Care. 2001;7(9):861–7.
- Chernew ME, Rosen AB, Fendrick AM. Value-Based Insurance Design. Health Affairs. 2007;26(2):w195–w203.
- University of Michigan Center for Value-Based Insurance Design [Internet]. [cited 2012 Nov 30]. Available from: http://vbidcenter.org/
- Goldman D, Joyce G, Zheng Y. Prescription Drug Cost Sharing: Associations With Medication And Medical Utilization And Spending And Health. Journal of the American Medical Association. 2007;298(1):61–9.
- Trivedi AN, Rakowski W, Ayanian JZ. Effect Of Cost Sharing On Screening Mammography In Medicare Health Plans. New England Journal of Medicine. 2008;358(4):375–83.
- Trivedi AN, Moloo H, Mor V. Increased Ambulatory Care Copayments And Hospitalizations Among The Elderly. New England Journal of Medicine. 2010;362(4):320-28.
- Congressional Budget Office Offsetting Effects Of Prescription Drug Use On Medicare’s Spending For Medical Services [Internet]. [cited 2012 Nov 30]. Available from: http://www.cbo.gov/publication/43741
- Fendrick AM, Jinnett K, Parry T. Synergies At Work: Realizing The Full Value Of Health Investments [Internet]. Integrated Benefits Institute, University of Michigan Center for Value-Based Insurance Design, National Pharmaceutical Council; 2011. [cited 2012 Nov 30]. Available from: http://www.npcnow.org/system/files/research/download/synergies_at_work_finalpaper.pdf
- Chourhry N, Fischer MA, Smith BF, et al. Five Features Of Value-Based Insurance Design Plans Were Associated With Higher Rates Of Medication Adherence. http://content.healthaffairs.org/content/early/2014/02/07/hlthaff.2013.0060.full.html
- Chernew ME, Shah MR, Wegh A, Rosenberg SN, Juster IA, Rosen AB, et al. Impact Of Decreasing Copayments On Medication Adherence Within A Disease Management Environment. Health Affairs. 2008;27(1):103–12.
- Maciejewski ML, Farley JF, Parker J, Wansink D. Copayment Reductions Generate Greater Medication Adherence In Targeted Patients. Health Affairs. 2010;29(11):2002-8.
- Choudhry NK, Avorn J, Glynn RJ, Antman EM, Schneeweiss S, Toscano M, et al. Full Coverage For Preventive Medications After Myocardial Infarction. New England Journal of Medicine. 2011;365(22):2088–97.
- Gibson TB, Mahoney J, Ranghell K, Cherney BJ, McElwee N. Value-Based Insurance Plus Disease Management Increased Medication Use And Produced Savings. Health Affairs. 2011;30(1):100–8.
- Kelly EJ, Turner CD, Frech-Tamas FH, Doyle JJ, Mauceri EG. Value-Based Benefit Design And Healthcare Utilization In Asthma, Hypertension, And Diabetes. American Journal of Pharmacy Benefits. 2009;1(4):217–21.
- Gibson TB, Wang S, Kelly E, Brown C, Turner C, Frech-Tamas F, et al. A Value-Based Insurance Design Program At A Large Company Boosted Medication Adherence For Employees With Chronic Illnesses. Health Affairs. 2011;30(1):109–17.
- Choudhry NK, Fischer MA, Avorn JL, Lee JL, Schneeweiss S, Solomon DH, et al. The Impact Of Reducing Cardiovascular Medication Copayments On Health Spending And Resource Utilization. Journal of the American College of Cardiology. 2012;60(18):1817–24.
- Shah ND, Naessens JM, Wood DL, Stroebel RJ, Litchy W, Wagie A, et al. Mayo Clinic Employees Responded To New Requirements For Cost Sharing By Reducing Possibly Unneeded Health Services Use. Health Affairs. 2011;30(11):2134–41.
- Kapowich JM. Oregon’s Test Of Value-Based Insurance Design In Coverage For State Workers. Health Affairs. 2010; 29(11):2028–32.
- Personal communication with JM Kapowich (Oregon Public Employees’ and Oregon Educators Benefit Boards), 27 Nov 2012.
- Fendrick AM, Smith DG, Chernew ME. Applying Value-Based Insurance Design To Low-Value Health Services. Health Affaris. 2010;29(11):2017-21.
- Pittman DG, Chen W, Bowlin SJ, Foody JM. Adherence To Statins, Subsequent Healthcare Costs, And Cardiovascular Hospitalizations. American Journal of Cardiology. 2011;107(11):1662–6.
- ABIM Foundation. Choosing Wisely [Internet]. [cited 2012 Nov 21]. Available from: http://www.abimfoundation.org/Initiatives/Choosing-Wisely.aspx
- Swinburn T, Ginsburg M, Benzik M, Clark R. Probing The Public’s Views On V-BID [Internet]. University of Michigan School of Public Health Center for Value-Based Insurance Design, Integrated Health Partners, Center for Healthcare Decisions; 2012. Available from: http://vbidcenter.org/wp-content/uploads/2014/08/VBID-ProbingthePublicsViewonVBID-Jun12.pdf
- Reischl TM, Morrel-Samuels S, Kusi C, Milkovich K, Benzik ME, Gingsburg M. Probing The Public’s Views On V-BID: Report II [Internet]. University of Michigan School of Public Health Prevention Research Center of Michigan, University of Michigan School of Public Health Center for Value-Based Insurance Design, Integrated Health Partners, Center for Healthcare Decisions; 2012. Available from: http://vbidcenter.org/wp-content/uploads/2014/08/VBID-Battle-Creek-II-FINAL.pdf
- Midwest Business Group on Health, University of Michigan Center for Value-Based Insurance Design, Buck Consultants. Communicating Value-Based Benefits Employee Research Project Results [Internet]. Midwest Business Group on Health, University of Michigan Center for Value-Based Insurance Design, Buck Consultants; 2012. Available from: http://vbidcenter.org/wp-content/uploads/2014/08/CommunicatingVBBenefits-Apr12.pdf
- Fairman KA, Curtiss FR. What Do We Really Know About VBID? Quality Of The Evidence And Ethical Considerations For Health Plan Sponsors. Journal of Managed Care Pharmacy. 2011;17(2):156–74.
- Lee JL, Maciejewski ML, Raju SS, Shrank WH, Choudhry NK. Value-Based Insurance Design: Quality Improvement But No Cost Savings. Health Affairs. 2013;32(7):1251–7.
- Maciejewski ML, Wansink D, Lindquist JH, Parker JC, Farley JF. Value-Based Insurance Design Program In North Carolina Increased Medication Adherence But Was Not Cost Neutral. Health Affairs. 2014;33(2):300–8.
- Chen S-Y, Shah SN, Lee Y-C, Boulanger L, Mardekian J, Kuznik A. Moving Branded Statins to Lowest Copay Tier Improves Patient Adherence. Journal of Managed Care Pharmacy. 2014;20(1):34–42.