Originally Produced: November 2013 Updated: July 2019
Protecting Preventive Care Coverage in the Post-ACA Era
Preventive Care Coverage in the ACA:
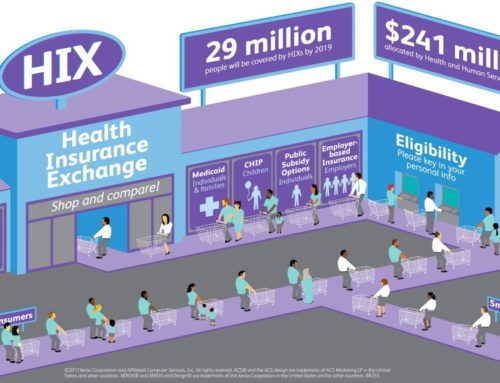
Section 2713 of the Public Health Service Act as amended by the Patient Protection and Affordable Care Act (ACA) requires that issuers offering group or individual health insurance plans must provide coverage for specified preventive services without a beneficiary copayment or a contribution toward a deductible. This elimination of consumer cost-sharing applies only when these services are delivered by a network provider.
Determining Covered Preventive Services:
Congress selected three organizations to determine covered preventive services with the intent to include all segments of the population. These organizations are the United States Preventive Services Task Force, the Centers for Disease Control and Prevention Advisory Committee on Immunization Practices, and the Health Resources and Services Administration. The current list of preventive services includes a variety of counseling services, immunizations, and screenings for cancer and treatable chronic diseases, such as diabetes and hypertension.
United States Preventive Services Task Force (USPSTF) is an independent body that does not necessitate approval from any Agency or Department before issuing a recommendation. The main responsibility of the USPSTF is to make recommendations on the use of primary preventive services through five level grades.
All services that receive an “A” or “B” rating from the USPSTF are defined as covered preventive services.
Advisory Committee on Immunization Practices (ACIP) is a group of medical and public health experts that develops recommendations on how to use vaccines to control diseases in the United States.
Immunization recommendations of the committee that have been adopted by the Director of the Centers for Disease Control and Prevention must be covered by applicable health plans.
Health Resources and Services Administration (HRSA) works to strengthen the health care workforce, build healthy communities, and improve health equity. The HRSA also works to provide health care to uninsured people, people living with HIV/AIDS, pregnant women, mothers, and children. The HRSA-supported women coverage guidelines, developed by the Institute of Medicine (IOM), ensure that women receive a comprehensive set of preventive services and fills gaps in other existing guidelines.
Women’s preventive health care – such as mammograms, screenings for cervical cancer, prenatal care, and other services – generally must be covered by health plans with no cost-sharing. However, the law recognizes the need to take into account the unique health needs of women throughout their lifespan.
Cost of care is explicitly not permitted in the selection of covered services. If a service is added to the covered services list, issuers have one calendar year from the date of the recommendation to include the new service without consumer cost-sharing. Services that are removed from the list are no longer required to be covered without cost-sharing by the issuer. However, to stay in compliance with other provisions in the ACA, the health plan is required to notify an enrollee 60 days before a co-payment, co-insurance, or deductible can be applied.[4]
Impact on Use of Preventive Services:
As of June 2019, 21 covered services have been identified for adults, 28 services for women (including pregnancy), and 31 services for children. Most of the recommendations are clinically nuanced, in that a specific population is clearly defined to receive each recommended service. Since the passage of the Affordable Care Act in 2010, the list of covered preventive services has been expanded to reflect current public health needs.
As of 2015, approximately 137 million Americans (108.8 million adults and 28.5 million children) received coverage for at least one free preventive service, such as a mammogram or flu shot.[5] Furthermore, utilization of preventive services is expected to increase as awareness of coverage grows. Currently, a significant number of Americans do not realize their preventive services are considered covered benefits under the ACA. [6] This may result in delay of care, poorer health outcomes, and more expensive health care.
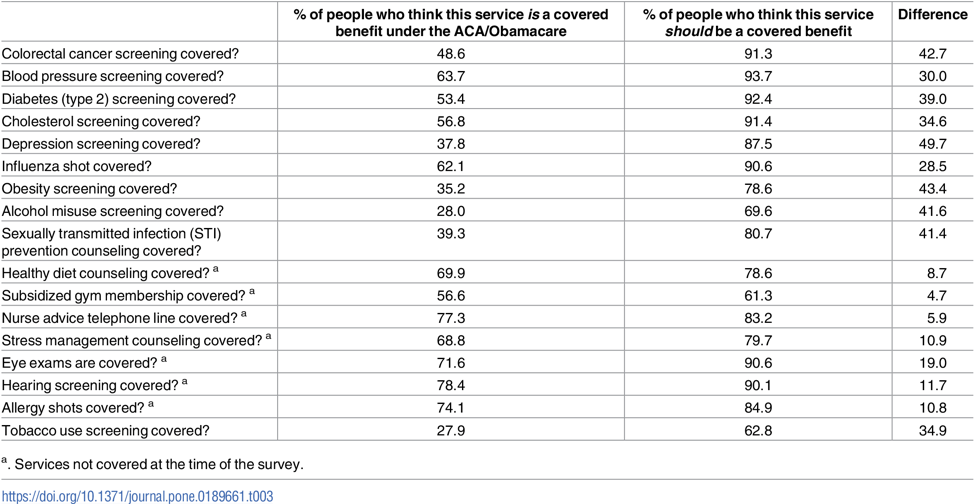
Benefits from the enhanced use of evidence-based preventive services are significant and well documented. A 2013 study published in the Journal of the American Board of Family Medicine found that changes in health insurance status were linked to preventive care consumption, which rose with coverage and fell without it.[2]
Conclusion
The ultimate test of health reform will be whether it expands coverage in a way that improves health and addresses rapidly rising costs. To build public support, efforts to bend the health care cost curve must be linked with a focus on patient-centered, high-quality care. By basing consumer cost-sharing on the health benefit – not the price – of services, clinically nuanced approaches such as Section 2713 of the ACA offer a promising opportunity to encourage clinically effective care by creating incentives for Americans to get the care they need.
The premise of Value-Based Insurance Design (V-BID) is to align consumer incentives with clinical evidence by reducing barriers to high-value services and providers (‘carrots’) and discouraging the use of low-value services and providers (‘sticks’). The V-BID model is driven by the concept of clinical nuance which recognizes that: 1) medical services differ in the benefit provided; and 2) the clinical benefit derived from a specific service depends on the patient using it, as well as when and where the service is provided.
While an increasing number of preventive services are being added to the list of covered services, many others remain the financial responsibility of the patient. Furthermore, these preventive screenings and tests may unfortunately detect serious chronic illnesses, and the associated treatments may have to be paid for out-of-pocket. This results in a contrariety between what is clinically valuable and what the patient will actually receive. By implementing V-BID principles moving forward, high value services, including chronic care, can be incorporated into this section of the ACA and continuity of care can be achieved.
References:
1 http://www.rwjf.org/content/dam/farm/reports/reports/2007/rwjf13325
2 http://jabfm.org/content/26/6/759.full
3 https://www.uspreventiveservicestaskforce.org/Page/Name/about-the-uspstf
4 http://www.gpo.gov/fdsys/pkg/FR-2010-07-19/pdf/2010-17242.pdf
6https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0189661